10+ Medcal Login Secrets For Faster Claims Processing

The healthcare industry has witnessed significant advancements in technology, leading to streamlined processes and improved patient care. One crucial aspect of healthcare administration is medical billing and claims processing. Efficient claims processing is vital for healthcare providers to receive timely reimbursements, which in turn, ensures the continuity of quality patient care. In this article, we will delve into the world of medical login secrets that can expedite claims processing, reducing the burden on healthcare staff and enhancing the overall efficiency of the system.
Understanding the Challenges in Claims Processing
Before we dive into the secrets of faster claims processing, it’s essential to understand the challenges that healthcare providers face. The claims process involves multiple stakeholders, including healthcare providers, patients, and insurance companies. Each stakeholder has its own set of requirements and protocols, which can lead to delays and discrepancies in the claims process. Some common challenges include:
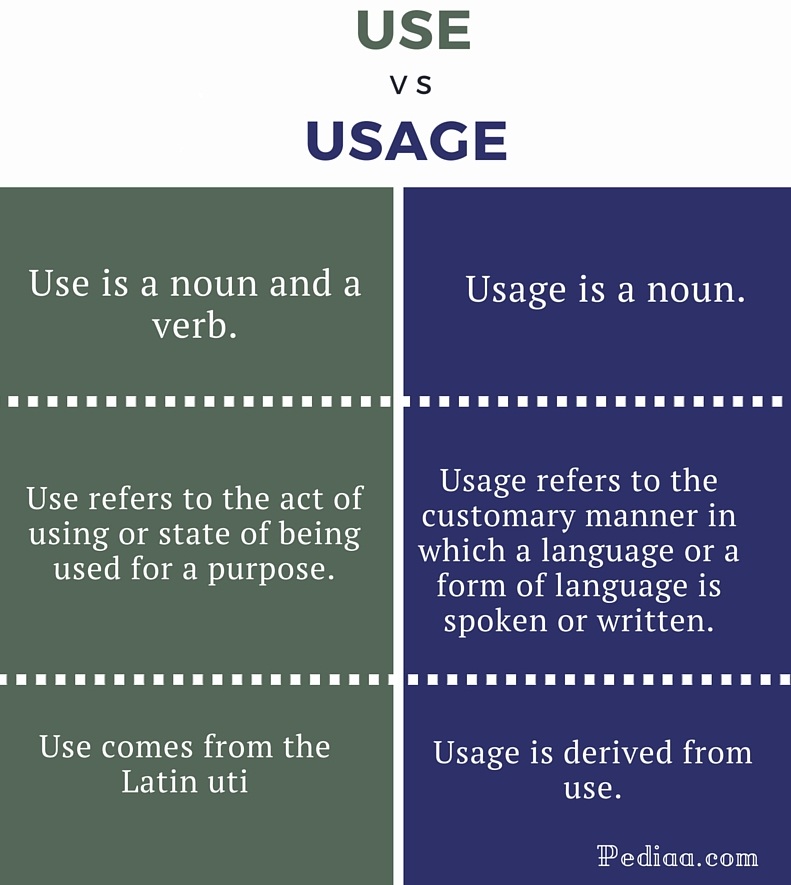
- Inaccurate or Incomplete Information: Claims are often rejected due to incorrect patient data, missing diagnosis codes, or incomplete treatment details.
- Complex Billing Codes: The use of incorrect or outdated billing codes can lead to claim rejections or underpayments.
- Manual Processing: Manual data entry and paper-based claims submission can be time-consuming and prone to errors.
Leveraging Technology for Efficient Claims Processing
Technology plays a pivotal role in modernizing the claims processing system. By adopting digital solutions, healthcare providers can significantly reduce the time and effort spent on claims processing. Some key technological advancements include:
- Electronic Health Records (EHRs): EHRs enable healthcare providers to access and manage patient data efficiently, reducing errors and improving data accuracy.
- Automated Billing Systems: These systems can generate claims automatically, using data from EHRs and practice management systems, thereby minimizing manual errors.
- Real-Time Eligibility Verification: This feature allows healthcare providers to verify patient eligibility and benefits in real-time, reducing the likelihood of claim rejections.
10+ Medical Login Secrets for Faster Claims Processing
Here are more than 10 medical login secrets and strategies that can help expedite claims processing:
- Implement a Secure and Efficient Claims Submission Process: Utilize a secure online portal for claims submission to ensure data integrity and reduce the risk of lost claims.
- Automate Claims Status Tracking: Leverage automated systems to track the status of claims, enabling prompt follow-up on pending claims and reducing the time spent on manual tracking.
- Use Data Analytics for Claims Processing Insights: Analyze claims data to identify trends, patterns, and areas for improvement, allowing for more informed decision-making.
- Streamline Patient Data Management: Implement a robust patient data management system to ensure accuracy and completeness of patient information, reducing claim rejections.
- Leverage Artificial Intelligence (AI) in Claims Processing: AI can help in automating tasks such as claims data entry, coding, and eligibility verification, improving efficiency and accuracy.
- Optimize Claims Denial Management: Implement a proactive approach to managing claims denials by identifying the root cause of denials and implementing corrective measures.
- Enhance Staff Training and Education: Ensure that billing and administrative staff are well-trained in claims processing best practices, coding, and compliance regulations.
- Utilize Real-Time Claims Adjudication: This feature enables healthcare providers to receive immediate feedback on claims status, facilitating prompt corrections and resubmissions.
- Implement a Patient Portal for Self-Service: Patient portals can empower patients to manage their own data, reducing administrative burdens and improving patient engagement.
- Engage in Regular Compliance Audits: Conduct regular audits to ensure compliance with regulatory requirements, reducing the risk of audits and penalties.
- Foster Strong Relationships with Payers: Building strong relationships with insurance payers can facilitate smoother claims processing and resolve issues more efficiently.
- Invest in Claims Processing Software: Utilize specialized software designed for claims processing to streamline tasks, improve accuracy, and enhance productivity.
Enhancing Claims Processing with Scenario-Based Examples
To illustrate the practical application of these medical login secrets, let’s consider a scenario:
Scenario: A healthcare provider submits a claim for a patient’s surgery, but the claim is rejected due to an incorrect billing code.
Solution: The healthcare provider can leverage automated billing systems to identify and correct the error. They can also use data analytics to track the frequency of similar errors and implement staff training to prevent future occurrences.
Creating a Culture of Efficiency and Compliance
Efficient claims processing is not just about adopting technology; it’s also about creating a culture of efficiency and compliance within the healthcare organization. This involves:
- Establishing Clear Policies and Procedures: Define and communicate clear policies and procedures for claims processing to ensure consistency and compliance.
- Encouraging Open Communication: Foster an environment where staff feel comfortable reporting errors or concerns, facilitating prompt corrective actions.
- Continuously Monitoring and Evaluating: Regularly assess claims processing efficiency and compliance, identifying areas for improvement and implementing necessary changes.
Implementing a Decision Framework for Informed Choices
When deciding on strategies to enhance claims processing, healthcare providers must make informed choices. A decision framework can help in evaluating options based on criteria such as:
- Cost-Effectiveness: Assess the financial impact of implementing new technologies or processes.
- Efficiency Gains: Evaluate the potential for increased productivity and reduced processing times.
- Compliance: Consider the regulatory implications and ensure that chosen strategies align with compliance requirements.
- Patient Satisfaction: Assess the potential impact on patient care and satisfaction.
Addressing Potential Objections or Limitations
One potential objection to implementing advanced claims processing technologies is the initial investment cost. However, it’s essential to weigh these costs against the long-term benefits of improved efficiency, reduced claim rejections, and enhanced patient care.
Frequently Asked Questions (FAQs)
What are the most common reasons for claim rejections?
+The most common reasons for claim rejections include inaccurate or incomplete patient data, incorrect billing codes, and lack of necessary documentation.
How can healthcare providers improve claims processing efficiency?
+Healthcare providers can improve claims processing efficiency by adopting automated billing systems, leveraging data analytics, and implementing staff training programs.
What role does technology play in modernizing claims processing?
+Technology plays a crucial role in modernizing claims processing by enabling the use of electronic health records, automated billing systems, and real-time eligibility verification, among other advancements.
How can healthcare providers ensure compliance with regulatory requirements?
+Healthcare providers can ensure compliance by conducting regular audits, providing ongoing staff training, and staying updated with the latest regulatory changes.
What is the importance of data analytics in claims processing?
+Data analytics is crucial in claims processing as it helps in identifying trends, patterns, and areas for improvement, enabling healthcare providers to make informed decisions.
How can patient portals enhance claims processing?
+Patient portals can empower patients to manage their own data, reducing administrative burdens and improving patient engagement, which in turn, can enhance claims processing efficiency.
Conclusion
In conclusion, the journey to faster claims processing is multifaceted, requiring a combination of technological adoption, process optimization, and cultural transformation. By understanding the challenges, leveraging technology, and implementing strategic medical login secrets, healthcare providers can significantly enhance the efficiency and accuracy of their claims processing. As the healthcare landscape continues to evolve, embracing these strategies will not only improve financial outcomes but also contribute to better patient care and satisfaction. By fostering a culture of compliance, efficiency, and patient-centricity, healthcare providers can navigate the complexities of claims processing with confidence, ensuring a smoother, more efficient experience for all stakeholders involved.