10+ Pancreatitis Causing Drugs You Should Avoid
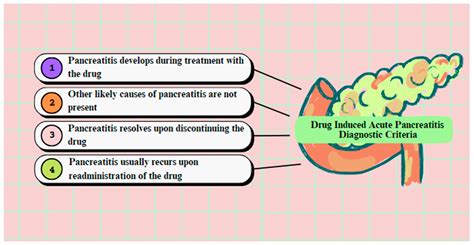
Pancreatitis, an inflammation of the pancreas, can be a painful and potentially life-threatening condition. While it is often associated with gallstones and excessive alcohol consumption, certain medications can also increase the risk of developing pancreatitis. It is essential to be aware of these pancreatitis-causing drugs to discuss alternative treatment options with your healthcare provider if necessary. Here’s a comprehensive overview of more than 10 drugs that have been linked to pancreatitis, along with a detailed explanation of the condition, its symptoms, diagnosis, treatment options, and prevention strategies.
Understanding Pancreatitis
Pancreatitis is a condition characterized by inflammation of the pancreas, a vital organ responsible for producing enzymes that aid in digestion and hormones that regulate blood sugar levels. There are two main types of pancreatitis: acute and chronic. Acute pancreatitis is a sudden inflammation of the pancreas, while chronic pancreatitis is a long-term inflammation that can lead to permanent damage.
Symptoms of Pancreatitis
The symptoms of pancreatitis can vary depending on the severity of the condition. Common symptoms include:
- Severe abdominal pain that radiates to the back
- Nausea and vomiting
- Fever
- Abdominal tenderness
- Rapid heart rate
- Swollen abdomen
Diagnosis of Pancreatitis
Diagnosing pancreatitis involves a combination of physical examination, medical history, and diagnostic tests. These tests may include:
- Blood tests to check for elevated levels of pancreatic enzymes
- Imaging tests such as CT scans or ultrasound to visualize the pancreas
- Endoscopic ultrasound to examine the pancreas and bile ducts
Treatment Options for Pancreatitis
Treatment for pancreatitis depends on the severity of the condition. Mild cases may be managed with supportive care, such as rest, hydration, and pain management. More severe cases may require hospitalization, antibiotics, and surgery to remove gallstones or repair damaged tissue.
Prevention Strategies
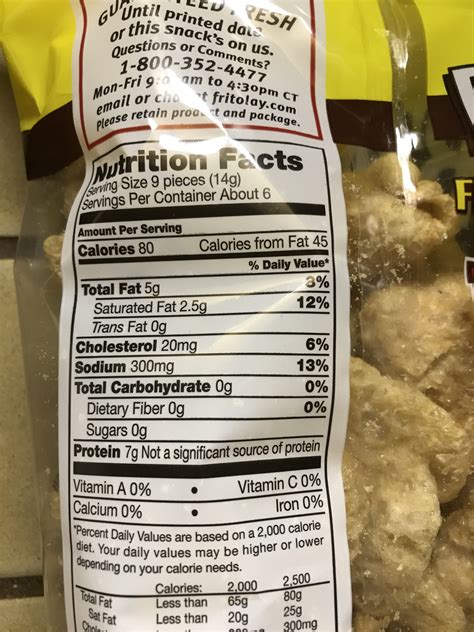
While some cases of pancreatitis cannot be prevented, there are steps you can take to reduce your risk. These include:
- Avoiding excessive alcohol consumption
- Maintaining a healthy weight
- Eating a balanced diet
- Avoiding certain medications that can increase the risk of pancreatitis
Drugs That Can Cause Pancreatitis
Here are over 10 drugs that have been associated with an increased risk of pancreatitis:
- Azathioprine: An immunosuppressive medication used to prevent organ rejection in transplant patients and to treat autoimmune diseases such as rheumatoid arthritis.
- Corticosteroids: A class of steroids that can cause hypertriglyceridemia, a condition characterized by high levels of triglycerides in the blood, which can increase the risk of pancreatitis.
- Valproic Acid: An anticonvulsant and mood stabilizer used to treat epilepsy, bipolar disorder, and migraines.
- Estrogen: Hormone replacement therapy (HRT) and certain birth control pills that contain estrogen can increase the risk of pancreatitis, particularly in women with a history of gallstones.
- Furosemide: A diuretic used to treat edema and high blood pressure, which can cause hypertriglyceridemia and increase the risk of pancreatitis.
- 6-Mercaptopurine: A chemotherapeutic agent used to treat certain types of cancer, such as leukemia, which can cause pancreatitis as a side effect.
- Didanosine: An antiretroviral medication used to treat HIV/AIDS, which has been linked to an increased risk of pancreatitis.
- Pentamidine: An antimicrobial medication used to treat and prevent pneumocystis pneumonia (PCP) in people with HIV/AIDS, which can cause pancreatitis as a side effect.
- Sulfonamides: A class of antibiotics that can cause hypertriglyceridemia and increase the risk of pancreatitis.
- Tamoxifen: A medication used to treat breast cancer, which can increase the risk of pancreatitis, particularly in women with a history of gallstones.
- Liraglutide: A medication used to treat type 2 diabetes, which has been linked to an increased risk of pancreatitis.
- Exenatide: A medication used to treat type 2 diabetes, which can increase the risk of pancreatitis, particularly when used in combination with other medications.
Case Study:
A 45-year-old woman with a history of gallstones was prescribed valproic acid for her epilepsy. After taking the medication for several months, she began to experience severe abdominal pain and was diagnosed with acute pancreatitis. Her healthcare provider immediately discontinued the valproic acid and switched her to an alternative medication. The patient made a full recovery and was able to manage her epilepsy without experiencing any further episodes of pancreatitis.
Future Trends Projection:
As the prevalence of pancreatitis continues to rise, it is essential to develop new treatments and prevention strategies. Researchers are currently exploring the use of genetic testing to identify individuals who may be at higher risk of developing pancreatitis. Additionally, new medications are being developed that can help reduce the risk of pancreatitis in people taking certain medications.
Pancreatitis is a serious condition that requires prompt medical attention. If you are experiencing symptoms such as severe abdominal pain, nausea, and vomiting, seek medical help immediately.
What to Do If You’re Taking These Medications
If you’re currently taking any of these medications and are concerned about your risk of pancreatitis, it’s essential to discuss your treatment options with your healthcare provider. They can help you weigh the benefits and risks of your medication and explore alternative treatment options if necessary. Additionally, it’s crucial to monitor your symptoms and seek medical attention immediately if you experience any signs of pancreatitis, such as severe abdominal pain, nausea, and vomiting.
What are the symptoms of pancreatitis?
+The symptoms of pancreatitis include severe abdominal pain, nausea, vomiting, fever, and abdominal tenderness. If you're experiencing any of these symptoms, seek medical attention immediately.
Can pancreatitis be prevented?
+While some cases of pancreatitis cannot be prevented, there are steps you can take to reduce your risk. These include avoiding excessive alcohol consumption, maintaining a healthy weight, eating a balanced diet, and avoiding certain medications that can increase the risk of pancreatitis.
What are the treatment options for pancreatitis?
+Treatment for pancreatitis depends on the severity of the condition. Mild cases may be managed with supportive care, such as rest, hydration, and pain management. More severe cases may require hospitalization, antibiotics, and surgery to remove gallstones or repair damaged tissue.
In conclusion, while certain medications can increase the risk of pancreatitis, it’s essential to discuss your treatment options with your healthcare provider to determine the best course of action for your specific medical condition. By being aware of the potential risks and taking steps to reduce your risk, you can help protect your pancreatic health and prevent this serious condition.