12+ Hcfa Claim Forms Secrets For Faster Payments
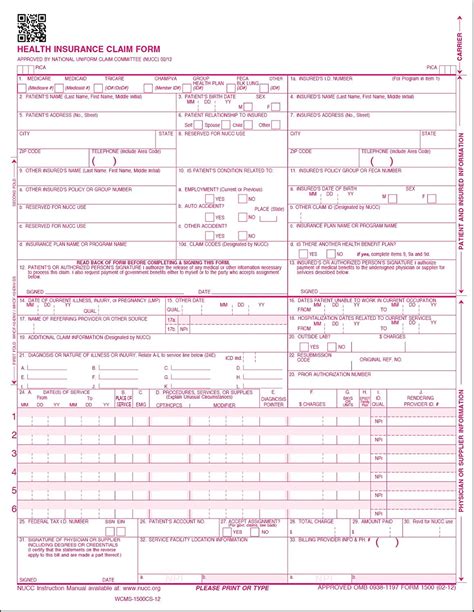
In the healthcare industry, the HCFA claim form, also known as the CMS-1500 form, is a crucial document used for billing and reimbursement purposes. The proper completion of this form is essential for healthcare providers to receive accurate and timely payments for their services. Over the years, the process of submitting claims has evolved, with advancements in technology and changes in regulations. However, the fundamental principles of completing an HCFA claim form remain a critical aspect of medical billing.
To streamline the reimbursement process and minimize delays, healthcare providers must understand the intricacies of the HCFA claim form. Here are 12+ secrets for faster payments, along with practical insights and explanations to help navigate the complexities of medical billing:
Accurate Patient Information: The foundation of a successful claim begins with accurate patient information. Ensure that the patient’s name, date of birth, address, and insurance details are correctly filled out. Any discrepancies can lead to claim denials or delays.
Correct Insurance Details: Provide the correct insurance information, including policy numbers, group numbers, and the name of the insurance company. This information is crucial for the claim to be processed correctly.
Use of Proper Codes: The use of correct medical codes is vital. Ensure that CPT (Current Procedural Terminology) and ICD-10 (International Classification of Diseases, 10th Revision) codes accurately reflect the services provided and the diagnoses.
Signature on File: Having a patient’s signature on file authorizing the release of medical information and assignment of benefits is essential. This can prevent delays in payment due to missing signatures.
Compliance with Regulations: Stay updated with the latest regulations and guidelines from the Centers for Medicare & Medicaid Services (CMS) and other regulatory bodies. Compliance is key to avoiding audits and ensuring smooth payment processes.
Electronic Claims Submission: Submitting claims electronically can significantly reduce processing time. Electronic claims are less prone to errors and can be transmitted quickly to payers.
Follow Up on Claims: Regular follow-up on submitted claims can help identify any issues promptly. This proactive approach ensures that any problems are addressed before they lead to significant delays.
Detailed Itemization: Clearly itemize all services provided on the claim form. This includes listing each procedure, medication, or supply, along with the corresponding codes and charges.
Use of Modifier Codes: Modifier codes provide additional information about the procedures performed. Correct use of these codes can prevent claim rejections and ensure accurate payment for services provided.
Timely Filing: Submit claims in a timely manner. Most payers have specific time limits for submitting claims, and late submissions can result in denied payments.
Verification of Benefits: Before rendering services, verify the patient’s benefits to understand what is covered and any out-of-pocket costs the patient may be responsible for. This can prevent unexpected denials or patient financial responsibilities.
Training and Education: Invest in ongoing training and education for billing staff. The healthcare billing landscape is constantly evolving, with updates to codes, regulations, and best practices. Well-trained staff are better equipped to handle the complexities of billing, leading to faster and more accurate payments.
Use of Technology: Leverage technology, such as billing software and automated systems, to streamline the billing process. These tools can help reduce errors, increase efficiency, and provide real-time tracking of claims.
Clear Communication: Maintain open and clear communication with patients, insurers, and other stakeholders. This includes explaining billing processes to patients, responding to inquiries from insurers, and keeping all parties informed about the status of claims.
By following these secrets and maintaining a commitment to accuracy, compliance, and efficiency, healthcare providers can significantly reduce the time it takes to receive payments for their services. In an industry where financial stability is crucial for delivering high-quality care, optimizing the billing process is not just a matter of administrative efficiency but also a key factor in ensuring the financial health of healthcare organizations.
Expert Insight: Implementing a comprehensive billing system that includes robust tracking and follow-up mechanisms can significantly improve payment turn-around times. Healthcare providers should also consider outsourcing their billing to professional medical billing companies if they lack the expertise or resources to manage the billing process efficiently in-house.
Common Challenges in HCFA Claim Forms
Despite the best efforts of healthcare providers, several challenges can arise when dealing with HCFA claim forms. These include:
- Denials Due to Incorrect Information: Claims can be denied due to incorrect patient or insurance information, emphasizing the need for accuracy in the billing process.
- Coding Errors: Mistakes in coding, such as using outdated codes or incorrect code combinations, can lead to claim rejections.
- Late Submissions: Failing to submit claims within the specified time frame can result in denied payments.
- Lack of Supporting Documentation: Insufficient or missing documentation to support the services billed can lead to audits or claim denials.
Strategies for Overcoming These Challenges
To overcome these challenges, healthcare providers can adopt several strategies:
- Implement Robust Quality Control Measures: Regularly review and verify the information on claim forms before submission to catch and correct errors.
- Invest in Ongoing Education and Training: Ensure that billing staff are up-to-date with the latest coding guidelines, regulatory changes, and best practices in medical billing.
- Utilize Technology: Leverage billing software and automated systems to streamline the billing process, reduce errors, and improve efficiency.
- Engage in Proactive Communication: Maintain open lines of communication with patients, insurers, and other stakeholders to address any issues promptly and prevent delays.
Step-by-Step Guide to Submitting an HCFA Claim Form
- Gather all necessary patient and insurance information.
- Verify benefits and ensure the patient's eligibility for services.
- Complete the claim form accurately, using correct codes and detailed itemization of services.
- Submit the claim electronically to expedite processing.
- Follow up on the claim status to address any issues promptly.
###Conclusion
The HCFA claim form is a vital tool in the medical billing process, serving as the primary means by which healthcare providers seek reimbursement for their services. By understanding the intricacies of this form and implementing strategies for accurate and efficient completion, healthcare providers can navigate the complexities of medical billing with greater ease. This not only ensures compliance with regulatory requirements but also facilitates smoother and faster payment processes, ultimately contributing to the financial stability and operational efficiency of healthcare organizations.
What is the significance of accurate patient information on the HCFA claim form?
+Accurate patient information is crucial for preventing claim denials and ensuring that payments are made correctly and efficiently. Incorrect or missing patient details can lead to delays or rejections of claims.
How can electronic claims submission benefit healthcare providers?
+Electronic claims submission can significantly reduce processing time, minimize errors, and provide faster payment turn-around times. It also reduces the administrative burden associated with manual claims processing.
What is the importance of ongoing education and training for billing staff?
+Ongoing education and training are essential for billing staff to stay updated with the latest coding guidelines, regulatory changes, and best practices in medical billing. This knowledge enables them to efficiently navigate the billing process, reducing errors and ensuring compliance.



