12 Heparin Induced Thrombocytopenia Facts For Safe Treatment

Heparin-induced thrombocytopenia (HIT) is a potentially life-threatening complication of heparin therapy, characterized by the formation of antibodies that activate platelets, leading to thrombocytopenia and thrombosis. It is crucial for healthcare professionals to be aware of the risks and management strategies associated with HIT to ensure safe and effective treatment. Here are 12 key facts about HIT that can guide clinicians in navigating this complex condition:
Pathophysiology: HIT is caused by the formation of antibodies against the complex of heparin and platelet factor 4 (PF4), which leads to the activation of platelets and the coagulation cascade. This results in both thrombocytopenia, due to platelet consumption, and a prothrombotic state.
Incidence: The incidence of HIT varies depending on the type of heparin used (unfractionated heparin vs. low molecular weight heparin), the duration of heparin therapy, and the patient population. Typically, it occurs in about 0.2% to 5% of patients treated with unfractionated heparin, with a higher incidence in surgical patients compared to medical patients.
Timing: HIT usually occurs between 5 to 14 days after the initiation of heparin therapy, although it can occur sooner if the patient has been exposed to heparin in the preceding 100 days. This timing is crucial for clinicians to monitor platelet counts and be vigilant for signs of thrombosis.
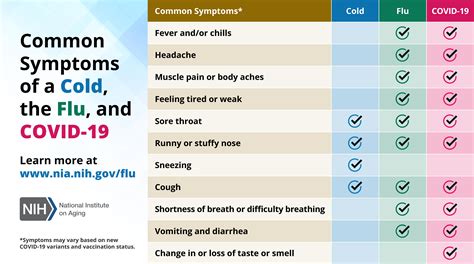
Clinical Presentation: The clinical presentation of HIT can vary widely, from asymptomatic thrombocytopenia to life-threatening thrombotic events such as deep vein thrombosis, pulmonary embolism, and even stroke. Some patients may experience skin necrosis at the site of heparin injection.
Diagnostic Criteria: The “4Ts” score is a useful tool for estimating the pre-test probability of HIT: Thrombocytopenia (platelet count fall), Timing (of thrombocytopenia in relation to heparin use), Thrombosis (occurrence of new thrombosis), and oTher causes of thrombocytopenia (absence of other evident causes). Laboratory tests, such as the PF4 enzyme-linked immunosorbent assay (ELISA) and functional assays like the serotonin release assay, are essential for confirming the diagnosis.
Treatment: The management of HIT involves immediate discontinuation of all forms of heparin and initiation of an alternative anticoagulant. Direct thrombin inhibitors (such as argatroban) and factor Xa inhibitors (such as fondaparinux) are commonly used. Warfarin should be avoided until platelet recovery has occurred and, even then, must be introduced with caution.
Thromboprophylaxis: In patients diagnosed with HIT, thromboprophylaxis is crucial to prevent new thrombotic events. This may involve the use of direct thrombin inhibitors or other non-heparin anticoagulants. The choice of agent depends on the patient’s renal function, the need for monitoring, and the specific clinical scenario.
Monitoring: Close monitoring of platelet counts is essential in patients suspected of having HIT. Both the absolute platelet count and the rate of decline are critical. Additionally, monitoring for signs of thrombosis and adjusting anticoagulation therapy as needed is vital.
Complications: The complications of HIT can be severe, including arterial and venous thrombi, limb loss, and death. Early recognition and treatment are critical in preventing these outcomes.
Re-exposure to Heparin: In patients with a history of HIT, re-exposure to heparin should be approached with caution. If heparin is necessary, it should be used for the shortest duration possible, and the patient should be closely monitored for signs of recurrent HIT.
Alternative Anticoagulants: The use of alternative anticoagulants has expanded the options for managing patients with HIT. These include direct oral anticoagulants (DOACs), which may offer a convenient alternative for long-term anticoagulation in some patients, although their use in HIT is still under investigation.
Prevention: Preventing HIT involves careful consideration of the risks and benefits of heparin therapy, the use of lower-risk alternatives when possible, and the implementation of protocols for monitoring and early detection of HIT in high-risk populations.
In conclusion, HIT is a serious condition that requires prompt recognition and management to prevent potentially catastrophic outcomes. By understanding the pathophysiology, clinical presentation, and treatment options for HIT, healthcare providers can deliver high-quality, patient-centered care that minimizes risks and maximizes benefits.
What is the primary cause of heparin-induced thrombocytopenia (HIT)?
+HIT is primarily caused by the formation of antibodies against the complex of heparin and platelet factor 4 (PF4), leading to platelet activation and a prothrombotic state.
How is HIT typically diagnosed?
+HIT is diagnosed based on clinical criteria (the “4Ts” score) and confirmed by laboratory tests such as the PF4 ELISA and functional assays like the serotonin release assay.
What is the appropriate initial treatment for HIT?
+The initial treatment for HIT involves the immediate discontinuation of all forms of heparin and the initiation of an alternative anticoagulant, such as a direct thrombin inhibitor or a factor Xa inhibitor.