12 Medications That Cause Pancreatitis Revealed

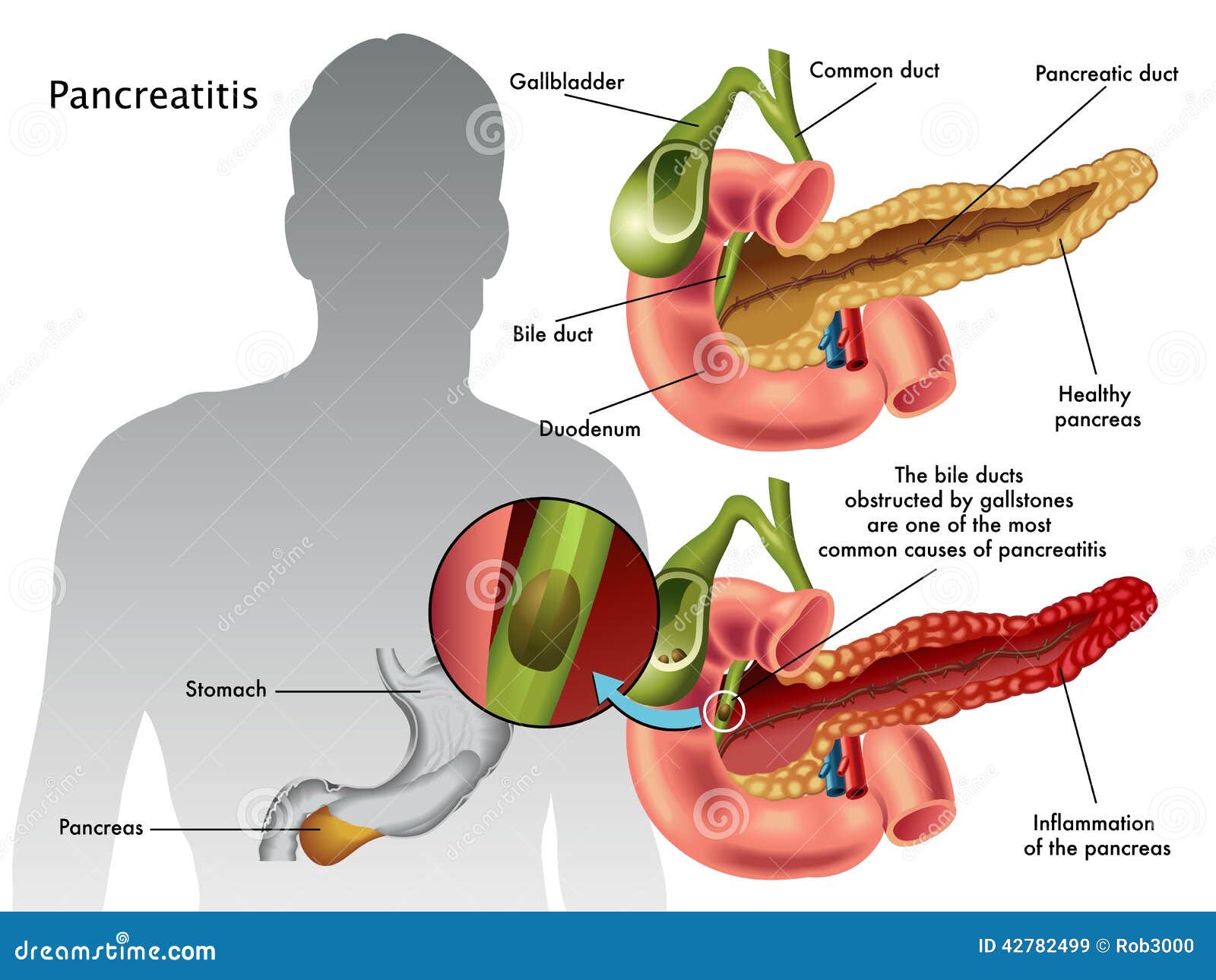
Pancreatitis, an inflammation of the pancreas, can be a painful and potentially life-threatening condition. While the exact cause of pancreatitis can vary, certain medications have been linked to an increased risk of developing this condition. Understanding which medications may contribute to pancreatitis is crucial for patients and healthcare providers alike, as it can inform medication choices and monitoring strategies. Here, we will delve into 12 medications that have been associated with pancreatitis, exploring their mechanisms, risks, and implications for patient care.
1. Azathioprine
Azathioprine is an immunosuppressive medication used to prevent the rejection of transplanted organs and to treat autoimmune diseases such as rheumatoid arthritis and Crohn’s disease. While effective, azathioprine has been linked to pancreatitis in some patients. The exact mechanism by which azathioprine causes pancreatitis is not fully understood, but it is believed to involve an allergic reaction or a direct toxic effect on the pancreas.
2. Valproic Acid
Valproic acid, commonly used to treat epilepsy, bipolar disorder, and to prevent migraine headaches, has a well-documented association with pancreatitis. The risk of pancreatitis with valproic acid is higher in children under the age of 2, and symptoms can develop anytime during treatment, from shortly after starting the medication to several years later.
3. L-asparaginase
L-asparaginase is a chemotherapy agent used primarily in the treatment of acute lymphoblastic leukemia (ALL). Pancreatitis is a recognized side effect of L-asparaginase, likely due to its effect on pancreatic enzymes and the induction of hypertriglyceridemia (high levels of triglycerides in the blood), which can also lead to pancreatitis.
4. Furosemide
Furosemide, a loop diuretic used to treat fluid build-up and swelling caused by congestive heart failure, liver cirrhosis, or a kidney disorder, can induce pancreatitis as an idiosyncratic reaction. The incidence is rare but highlights the importance of monitoring for signs of pancreatitis in patients on long-term diuretic therapy.
5. Estrogen
Estrogen therapy, including oral contraceptives and hormone replacement therapy (HRT), has been associated with an increased risk of pancreatitis, particularly when combined with other factors like hypertriglyceridemia. Estrogen can increase the levels of triglycerides in the blood, thereby elevating the risk of developing pancreatitis.
6. 6-Mercaptopurine
6-Mercaptopurine, a medication used to treat certain types of cancer and autoimmune diseases, has been linked to pancreatitis. This drug metabolite can cause damage to the pancreas, leading to inflammation, although the risk is considered relatively low.
7. Pentamidine
Pentamidine, an antiprotozoal and antifungal medication, is used to treat and prevent Pneumocystis jirovecii pneumonia (PCP) in patients with HIV/AIDS. One of the side effects of pentamidine is pancreatitis, which may occur more frequently when the drug is administered parenterally.
8. Didanosine
Didanosine, an antiretroviral medication used in the treatment of HIV/AIDS, has been associated with pancreatitis. The risk is significant enough that patients on didanosine should be closely monitored for signs of pancreatitis, such as abdominal pain, nausea, and vomiting.
9. Simvastatin
Simvastatin, a statin used to lower cholesterol, has been rarely associated with pancreatitis. While the evidence is not as strong as with some other medications, the potential link highlights the need for continued monitoring and reporting of adverse effects associated with all medications.
10. Mesalamine
Mesalamine, a medication used to treat ulcerative colitis and Crohn’s disease, is designed to reduce inflammation in the digestive tract. However, it has been associated with pancreatitis in rare instances, possibly due to an idiosyncratic reaction or as part of a hypersensitivity reaction.
11. Corticosteroids
Corticosteroids, especially when used in high doses or for prolonged periods, can contribute to the development of pancreatitis, primarily through the promotion of hypertriglyceridemia. The risk may be elevated in patients with pre-existing liver disease or other metabolic disorders.
12. Tetracyclines
Tetracyclines, a class of antibiotics used to treat various infections, have been linked to pancreatitis, particularly minocycline. The mechanism is not fully understood but is thought to involve an allergic or idiosyncratic reaction rather than a direct toxic effect.
Understanding the Risk
While these medications have been associated with pancreatitis, it’s essential to understand that the risk varies from one medication to another and from one individual to another. Patients should not stop taking their prescribed medications without consulting their healthcare provider, as the benefits of these drugs often outweigh the risks for most people.
Prevention and Monitoring
Preventing pancreatitis in patients taking these medications involves regular monitoring for signs and symptoms, such as severe abdominal pain, nausea, vomiting, and changes in stool. Additionally, managing risk factors like high triglycerides and monitoring pancreatic enzymes can help in early detection.
Conclusion
Medications can be a significant cause of pancreatitis, and recognizing these potential risks is crucial for effective patient management. By understanding the medications that can lead to pancreatitis and through vigilant monitoring and early detection, healthcare providers can mitigate these risks and ensure the best possible outcomes for their patients.
What are the symptoms of pancreatitis?
+Symptoms of pancreatitis can include severe abdominal pain that may radiate to the back, nausea, vomiting, fever, and changes in stool or urine output. In severe cases, symptoms can progress to include difficulty breathing, rapid heart rate, and even shock.
How is pancreatitis diagnosed?
+Diagnosis of pancreatitis typically involves a combination of physical examination, medical history, and diagnostic tests such as blood tests to check for elevated pancreatic enzymes (amylase and lipase), imaging tests like CT scans or ultrasound to visualize the pancreas, and sometimes endoscopic procedures.
Can pancreatitis be treated?
+Treatment of pancreatitis depends on its severity and may include hospitalization for supportive care such as intravenous fluids, pain management, and bowel rest. In mild cases, treatment may be managed on an outpatient basis. For chronic pancreatitis, management may involve pain control, pancreatic enzyme replacement, and dietary modifications.
By knowing the medications that can cause pancreatitis and understanding the preventive measures and treatment options, individuals can better navigate their health care, ensuring they receive the most effective treatment while minimizing risks.