12+ Ondansetron Tips For Effective Vomiting Control
Vomiting, a common and distressing symptom, can be caused by a variety of factors including chemotherapy, radiation therapy, surgery, and gastrointestinal infections. Ondansetron, a selective serotonin 5-HT3 receptor antagonist, has emerged as a highly effective antiemetic medication for controlling vomiting. First approved by the FDA in 1991, ondansetron has been widely used in clinical settings for its ability to prevent nausea and vomiting associated with cancer chemotherapy, radiation therapy, and surgery.
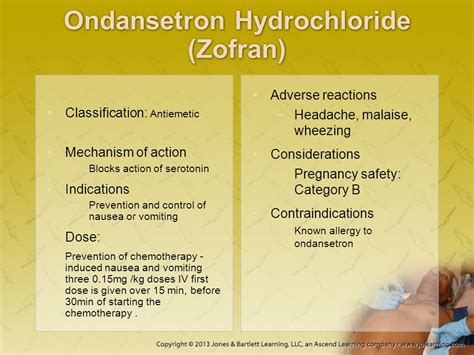
Understanding Ondansetron
ToHarness the full potential of ondansetron, it’s crucial to understand its mechanism of action. By blocking the action of serotonin, a natural substance that may cause nausea and vomiting, ondansetron effectively prevents the vomiting reflex. This understanding forms the basis of its use in managing acute and delayed nausea and vomiting caused by chemotherapy and radiation therapy, as well as postoperative nausea and vomiting.
Effective Administration
- Timing is Everything: Administering ondansetron 30 minutes before chemotherapy or radiation therapy can significantly enhance its efficacy. For surgery, administering it before the procedure or immediately after can be beneficial.
- Dosing: The dosage and frequency of administration can vary depending on the cause of vomiting and the patient’s response. Typically, for chemotherapy-induced nausea and vomiting, a dose of 8mg is given 30 minutes before chemotherapy, followed by 8mg every 8 hours for up to 2 days after chemotherapy.
- Combination Therapy: Often, ondansetron is more effective when used in combination with other antiemetic agents, such as dexamethasone. This multi-modal approach can provide comprehensive coverage against both acute and delayed emesis.
Key Considerations
- Age and Renal Impairment: Dose adjustments may be necessary for elderly patients and those with severe hepatic impairment. Monitoring renal function is also crucial, especially in patients with pre-existing kidney issues.
- Drug Interactions: Ondansetron can interact with other medications, including warfarin, and certain medications that affect the liver enzymes. Close monitoring and potential dose adjustments of the interacting medications may be necessary.
Side Effects and Management
While ondansetron is generally well-tolerated, side effects can include headache, constipation, and injection site reactions. In rare cases, it can cause serious side effects such as serotonin syndrome, especially when taken with other serotonergic drugs.
Patient Education
Educating patients on how to take ondansetron, including the timing and dosing, is vital for its effectiveness. Additionally, informing patients about potential side effects and the importance of reporting them can improve compliance and outcomes.
Emerging Trends and Future Directions
Research into the antiemetic effects of ondansetron continues, with ongoing studies examining its efficacy in combination with newer agents and its potential role in managing nausea and vomiting in other clinical contexts, such as during pregnancy or in palliative care settings.
Case Study: Ondansetron in Chemotherapy-Induced Nausea and Vomiting
A significant body of evidence supports the use of ondansetron in chemotherapy-induced nausea and vomiting (CINV). A study comparing ondansetron with metoclopramide in patients receiving cisplatin chemotherapy demonstrated a higher complete response rate (no vomiting, no rescue medication) with ondansetron, highlighting its efficacy in this patient population.
Comparative Analysis: Ondansetron vs. Other Antiemetics
Comparative studies between ondansetron and other serotonin antagonists, such as granisetron and tropisetron, have shown varying degrees of efficacy. While ondansetron remains a gold standard, newer agents like palonosetron offer prolonged action and may provide additional benefits in certain patient groups, particularly in preventing delayed emesis.
Technical Breakdown: Pharmacokinetics of Ondansetron
Understanding the pharmacokinetics of ondansetron, including its absorption, distribution, metabolism, and excretion, can provide insights into its dosing and potential drug interactions. Ondansetron is absorbed rapidly after oral administration, with bioavailability affected by factors such as food intake and liver function.
Myth vs. Reality: Separating Facts from Fiction
Despite its widespread use, several misconceptions surround ondansetron. For instance, the belief that it is only effective for chemotherapy-induced nausea is a myth; it has proven efficacy in a range of vomiting causes. Another misconception is that it completely eliminates nausea and vomiting in all patients, which is not the case. Individual responses can vary, and some patients may still experience breakthrough nausea or vomiting, necessitating additional treatment strategies.
Resource Guide: Additional Tools for Vomiting Control
For comprehensive management of vomiting, healthcare providers can utilize a range of additional tools and resources: - Guidelines and Protocols: Adhering to established clinical guidelines for antiemetic use can help standardize care and improve outcomes. - Patient Support Groups: Connecting patients with support groups can provide emotional support and practical advice for managing side effects. - Medication Management Apps: Utilizing apps that help track medication schedules and dosages can improve adherence and reduce the risk of side effects.
Decision Framework: Selecting the Right Antiemetic Regimen
When selecting an antiemetic regimen, healthcare providers should consider several factors, including the cause of vomiting, the patient’s medical history, potential drug interactions, and the efficacy and safety profile of available antiemetics. A tailored approach that addresses individual patient needs can optimize vomiting control and improve quality of life.
Conceptual Exploration: The Future of Vomiting Control
The future of vomiting control may involve the development of newer, more targeted antiemetic agents, as well as innovative delivery systems designed to enhance bioavailability and patient compliance. Additionally, there may be a greater emphasis on personalized medicine approaches, where antiemetic therapy is tailored to the individual’s genetic predisposition, medical history, and response to therapy.
FAQ Section
What is the most effective dose of ondansetron for preventing chemotherapy-induced nausea and vomiting?
+The most effective dose of ondansetron can vary, but a common regimen is 8mg administered 30 minutes before chemotherapy, followed by 8mg every 8 hours for up to 2 days after chemotherapy.
Can ondansetron be used in combination with other antiemetic medications?
+Yes, ondansetron is often used in combination with other antiemetic agents, such as dexamethasone, to provide comprehensive coverage against both acute and delayed emesis.
Are there any potential drug interactions with ondansetron that I should be aware of?
+Ondansetron can interact with other medications, including warfarin, and medications that affect the liver enzymes. Close monitoring and potential dose adjustments of the interacting medications may be necessary.
Can ondansetron cause any serious side effects?
+While rare, ondansetron can cause serious side effects such as serotonin syndrome, especially when taken with other serotonergic drugs. Monitoring for these side effects and reporting them promptly to healthcare providers is crucial.
Is ondansetron effective for all types of vomiting?
+Ondansetron is highly effective for chemotherapy-induced and postoperative nausea and vomiting but may not be equally effective for all types of vomiting. Individual responses can vary, and other causes of vomiting may require different treatment approaches.
In conclusion, ondansetron remains a cornerstone in the management of vomiting, particularly in the contexts of chemotherapy and postoperative settings. Its effectiveness, combined with a generally favorable safety profile, makes it a preferred choice among healthcare providers. However, recognizing the complexity of vomiting control and the need for individualized treatment strategies is essential for optimizing patient outcomes. As research continues to evolve, the future of vomiting control promises to be more personalized and effective, offering hope for improved quality of life for those affected by this distressing symptom.