Abdominal Aortic Aneurysm Surgery
Abdominal aortic aneurysm (AAA) surgery is a complex and highly specialized medical procedure aimed at repairing or replacing the aorta, the largest blood vessel in the body, when it becomes weakened and balloons out, forming an aneurysm. This condition is life-threatening if left untreated, as the aneurysm can rupture, leading to severe internal bleeding that is often fatal. The surgery for AAA has evolved significantly over the years, offering patients various treatment options depending on the size, location, and overall health of the individual.
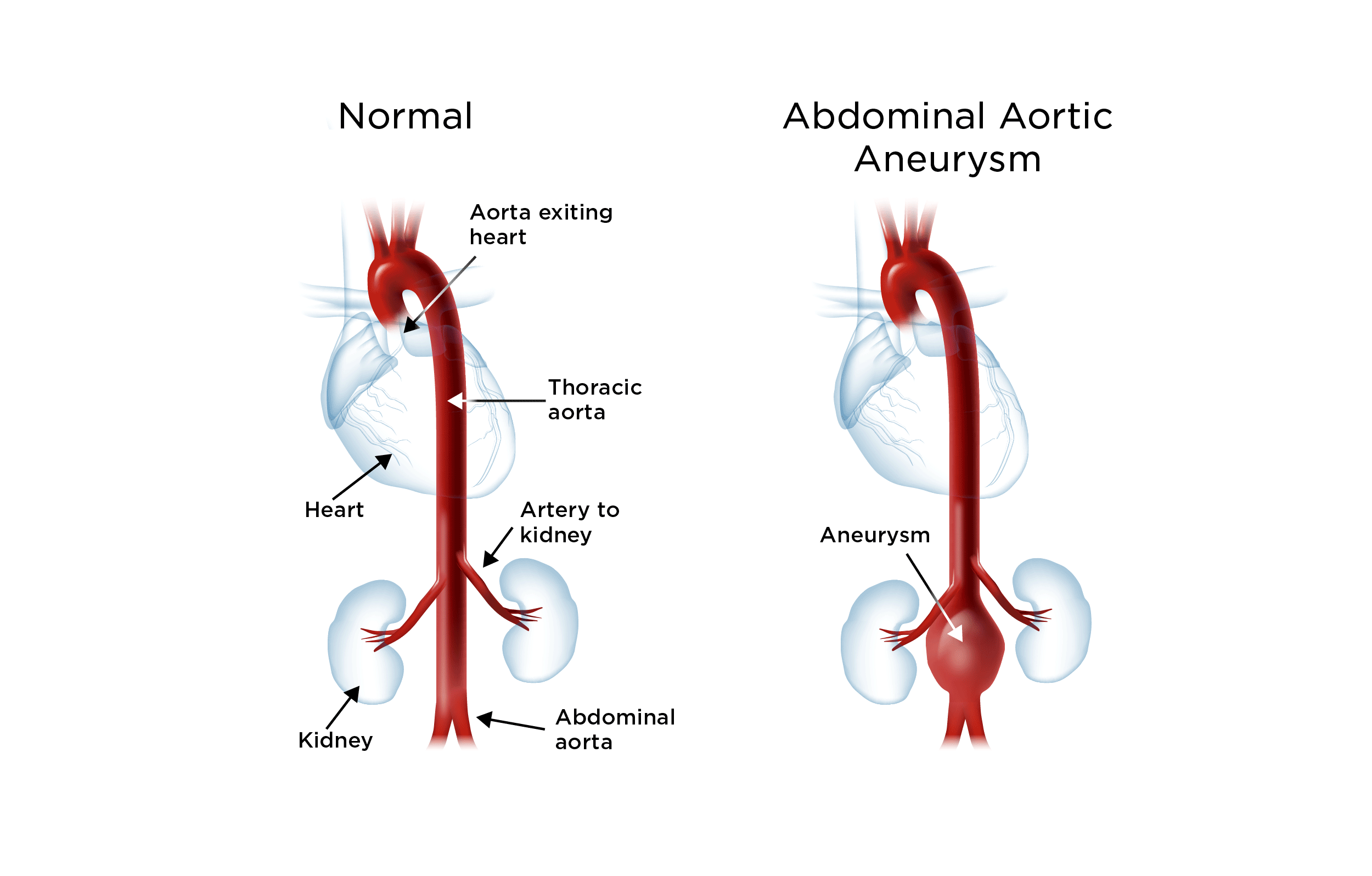
Understanding Abdominal Aortic Aneurysms
An abdominal aortic aneurysm occurs when the lower part of the aorta, which runs through the abdomen, weakens and bulges. The most common cause is atherosclerosis, a condition in which plaque builds up inside the arteries, weakening the walls. High blood pressure, smoking, and genetics can also contribute to the development of an AAA. Small aneurysms might not cause symptoms and may be monitored with regular ultrasound checks. However, as the aneurysm grows, it can put pressure on the surrounding structures, leading to symptoms such as abdominal pain, back pain, or a palpable mass in the abdomen. The risk of rupture increases with the size of the aneurysm, necessitating surgical intervention once it reaches a certain diameter, typically around 5.5 cm.
Surgical Options for AAA Repair
There are primarily two types of surgical approaches for repairing an abdominal aortic aneurysm: open repair and endovascular aneurysm repair (EVAR).
Open Repair
Open repair is the traditional method used for AAA surgery. It involves a major surgical incision in the abdomen to access the aorta. The surgeon then clamps the aorta above and below the aneurysm, opens the aneurysm, and sews a graft into place to replace the weakened section of the aorta. The graft is typically made of a durable, woven material that the body tolerates well. This method is highly effective but comes with significant risks and a longer recovery period compared to EVAR. It’s often chosen for patients who are good surgical candidates and when the anatomy of the aneurysm is not suitable for EVAR.
Endovascular Aneurysm Repair (EVAR)
EVAR is a minimally invasive procedure that has become increasingly popular for treating AAAs. It involves making small incisions in the groin to insert catheters that guide and deploy a stent-graft through the arteries to the aortic aneurysm. The stent-graft is then expanded to fit snugly against the aorta, both above and below the aneurysm, ensuring that blood flows through the graft and not into the aneurysm. This approach reduces recovery time significantly and is generally preferred for patients who are at higher risk for open surgery due to other health issues. However, not all patients are candidates for EVAR, and the long-term durability of the stent-graft is a consideration.
Decision Framework for Surgical Approach
The decision between open repair and EVAR depends on several factors, including the size and location of the aneurysm, the patient’s overall health, age, and other medical conditions. A multidisciplinary team, including vascular surgeons, radiologists, and other specialists, will evaluate these factors to determine the most appropriate treatment plan.
- Patient Health: Patients with significant co-morbidities may be better candidates for EVAR due to its less invasive nature.
- Aneurysm Characteristics: The shape, size, and location of the aneurysm, as well as its proximity to vital branches of the aorta, play a crucial role in deciding the surgical approach.
- Risk of Rupture: The risk of rupture versus the risks associated with surgery must be carefully weighed, especially for smaller aneurysms.
Post-Surgical Care and Recovery
After AAA surgery, whether open or endovascular, close monitoring is necessary to watch for potential complications such as bleeding, infection, or issues related to the graft. Patients typically spend several days in the hospital after open repair and less time after EVAR. A period of recovery at home follows, during which heavy lifting, bending, and strenuous activities should be avoided. Follow-up appointments with the surgeon and imaging tests are crucial to ensure the graft is functioning properly and the aneurysm is not growing.
Emerging Trends and Future Directions
Advancements in surgical techniques, imaging technologies, and device development continue to improve outcomes for patients with abdominal aortic aneurysms. For instance, fenestrated and branched EVAR devices now allow for the treatment of more complex aneurysms that involve the branches of the aorta, which was previously a challenge. Moreover, research into the genetic and molecular underpinnings of aneurysm formation may lead to novel therapeutic approaches aimed at preventing or slowing the growth of aneurysms.
FAQ Section
What are the risks associated with untreated abdominal aortic aneurysms?
+The primary risk of an untreated abdominal aortic aneurysm is rupture, which can lead to severe internal bleeding and is often fatal. Early detection and treatment are crucial to prevent such outcomes.
How do I know if I'm a candidate for endovascular aneurysm repair (EVAR)?
+Candidacy for EVAR is determined on an individual basis, considering factors such as the aneurysm's size, location, and shape, as well as the patient's overall health and anatomy. A thorough evaluation by a vascular specialist is necessary to determine the best treatment option.
What is the typical recovery time after AAA surgery?
+Recovery time varies significantly between open repair and EVAR. Open repair typically requires several weeks to a few months for full recovery, while EVAR patients often recover within a few weeks. However, individual recovery times can vary based on overall health, age, and the presence of other medical conditions.
In conclusion, abdominal aortic aneurysm surgery represents a critical intervention for a potentially lethal condition. The advancement in surgical techniques and technologies has expanded treatment options, offering hope for improved outcomes and quality of life for patients. Continuing research and advancements in the field are expected to further refine these treatments, aiming for even better results in the management of AAA.



