Abo Rhesus Blood Group
The ABO blood group system is one of the most important blood types in human beings, and it’s named after the first three letters of the words “AB” and “O”. This system is crucial for transfusion medicine, as it determines the compatibility of blood between donors and recipients. In this article, we’ll delve into the specifics of the ABO blood group system, with a special focus on the Rhesus blood group system, which is also known as the Rh system.
The ABO blood group system was first discovered in 1901 by Austrian physician Karl Landsteiner, who found that human blood could be classified into three main groups: A, B, and O. Later, in 1910, Landsteiner and Alfred von Decastello discovered the AB blood group, which is a combination of the A and B antigens. The ABO blood group system is controlled by a single gene with three alleles: A, B, and O. The A and B alleles are codominant, while the O allele is recessive.
The Rhesus blood group system, on the other hand, was discovered in 1940 by Karl Landsteiner and Alexander S. Wiener, who found that the blood of Rhesus monkeys could be used to induce an immune response in human beings. The Rh system is also known as the Rhesus D antigen, and it’s found on the surface of red blood cells. If an individual has the Rh antigen, they’re considered Rh-positive, while those without it are considered Rh-negative. The Rh system is also controlled by a single gene with two alleles: RHD and RHDnull.
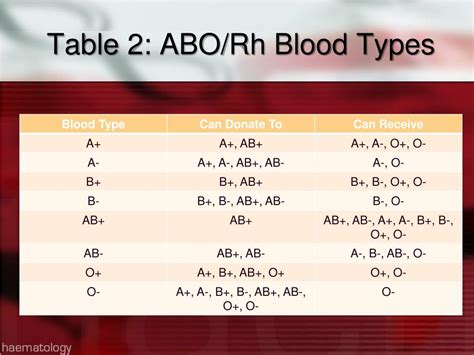
The combination of the ABO and Rh systems gives us eight possible blood types: A+, A-, B+, B-, AB+, AB-, O+, and O-. The “+” and “-” symbols indicate the presence or absence of the Rh antigen. The distribution of these blood types varies among different populations, with the most common being O+ and A+, followed by B+ and AB+. The rarest blood type is AB-, found in less than 1% of the population.
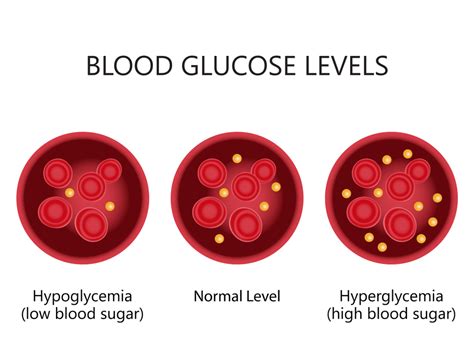
Understanding the ABO and Rh blood group systems is crucial for ensuring safe blood transfusions. If an individual receives blood from a donor with an incompatible blood type, it can lead to a severe hemolytic reaction, which can be life-threatening. For example, if an Rh-negative individual receives blood from an Rh-positive donor, their immune system may react to the Rh antigen, leading to the production of antibodies that can attack the transfused red blood cells.
To avoid such complications, blood banks and transfusion services use a rigorous testing process to ensure compatibility between donors and recipients. This includes testing for the ABO and Rh blood groups, as well as other antigens that may be present on the surface of red blood cells. Additionally, individuals with rare blood types, such as AB-, may need to undergo more extensive testing to ensure compatibility with available blood supplies.
In addition to their importance in transfusion medicine, the ABO and Rh blood group systems have also been studied for their potential associations with various diseases and conditions. For example, research has suggested that individuals with certain ABO blood types may be more susceptible to certain infections, such as cholera or gastric ulcers. Similarly, the Rh system has been linked to an increased risk of certain autoimmune disorders, such as rheumatoid arthritis.
While the ABO and Rh blood group systems are well understood, there’s still much to be learned about the genetics and molecular mechanisms that control these systems. Ongoing research is focused on developing new technologies and strategies for blood typing, as well as improving our understanding of the complex interactions between the immune system and red blood cells.
In conclusion, the ABO and Rh blood group systems play a critical role in ensuring safe blood transfusions and are an essential part of our understanding of human genetics and immunology. By continuing to study and learn about these systems, we can develop new and innovative approaches to improving patient care and saving lives.
What is the most common blood type?
+The most common blood type is O+, found in approximately 37.4% of the population, followed closely by A+, which is found in around 33.7% of individuals.
Can I change my blood type?
+No, it's not possible to change your blood type. The ABO and Rh blood group systems are determined by your genetic makeup and are fixed at birth.
What happens if I receive blood from a donor with an incompatible blood type?
+Receiving blood from a donor with an incompatible blood type can lead to a severe hemolytic reaction, which can be life-threatening. This is because your immune system may react to the transfused red blood cells, leading to the production of antibodies that can attack and destroy them.
Understanding the ABO and Rh blood group systems is crucial for ensuring safe blood transfusions. By continuing to study and learn about these systems, we can develop new and innovative approaches to improving patient care and saving lives.
The study of the ABO and Rh blood group systems has come a long way since their discovery, and it continues to be an active area of research. As we learn more about the genetics and molecular mechanisms that control these systems, we can develop new and innovative approaches to improving patient care and saving lives. Whether you’re a medical professional, a researcher, or simply someone interested in learning more about the human body, the ABO and Rh blood group systems are an essential part of our understanding of human genetics and immunology.
In the future, we can expect to see continued advancements in our understanding of the ABO and Rh blood group systems, as well as the development of new technologies and strategies for blood typing. This may include the use of machine learning algorithms to improve blood matching, or the development of new treatments for individuals with rare blood types. Whatever the future holds, one thing is certain: the study of the ABO and Rh blood group systems will continue to play a critical role in improving patient care and saving lives.
Understanding the ABO Blood Group System: A Step-by-Step Guide
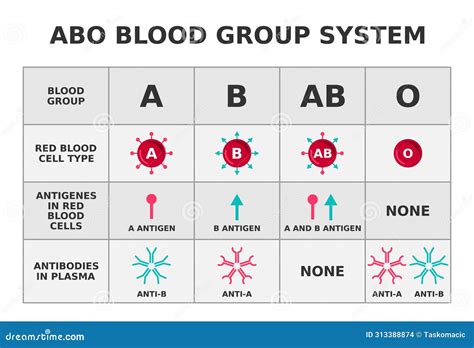
- Learn about the three main ABO blood groups: A, B, and O.
- Understand how the ABO blood group system is controlled by a single gene with three alleles: A, B, and O.
- Discover how the A and B alleles are codominant, while the O allele is recessive.
- Learn about the different ABO blood types, including A+, A-, B+, B-, AB+, AB-, O+, and O-.
- Understand the importance of ABO blood typing in transfusion medicine.
In addition to the ABO blood group system, the Rh blood group system is also an essential part of our understanding of human genetics and immunology. The Rh system is controlled by a single gene with two alleles: RHD and RHDnull. Individuals with the Rh antigen are considered Rh-positive, while those without it are considered Rh-negative.
The combination of the ABO and Rh systems gives us eight possible blood types, each with its own unique characteristics and requirements. Understanding these blood types is crucial for ensuring safe blood transfusions, as receiving blood from a donor with an incompatible blood type can lead to a severe hemolytic reaction.
In conclusion, the ABO and Rh blood group systems are complex and fascinating topics that continue to be an active area of research. By continuing to study and learn about these systems, we can develop new and innovative approaches to improving patient care and saving lives. Whether you’re a medical professional, a researcher, or simply someone interested in learning more about the human body, the ABO and Rh blood group systems are an essential part of our understanding of human genetics and immunology.
The Pros and Cons of Blood Typing

Pros:
- Ensures safe blood transfusions
- Helps to prevent severe hemolytic reactions
- Allows for the identification of rare blood types
Cons:
- Can be time-consuming and expensive
- May require specialized equipment and training
- Can be limited by the availability of blood typing reagents