Amlodipine Uses Explained: Benefits Uncovered
Amlodipine, a calcium channel blocker, has been a cornerstone in the management of hypertension and angina pectoris for decades. Its efficacy in reducing blood pressure and alleviating chest pain has made it a widely prescribed medication globally. However, the benefits of amlodipine extend beyond its primary uses, and understanding its mechanisms and applications can provide valuable insights into its therapeutic potential.
Historical Evolution of Amlodipine
First approved by the FDA in 1992, amlodipine was introduced as a novel therapeutic agent for the treatment of hypertension and angina. Its development marked a significant advancement in the field of cardiovascular medicine, offering a new approach to managing conditions that were previously challenging to treat. Over the years, extensive research has elucidated the pharmacodynamics and pharmacokinetics of amlodipine, contributing to its widespread acceptance as a first-line treatment for various cardiovascular diseases.
Technical Breakdown: How Amlodipine Works
Amlodipine operates by inhibiting the influx of calcium ions into vascular smooth muscle cells and cardiac muscles. This action dilates peripheral and coronary blood vessels, reducing vascular resistance and increasing oxygen supply to the myocardium. The resultant decrease in blood pressure and reduction in cardiac afterload contribute to its therapeutic effects in hypertension and angina. Furthermore, amlodipine’s mechanism of action is characterized by its high lipid solubility, which allows it to Cross biological membranes easily, and its slow onset of action, which enables once-daily dosing and enhances patient compliance.
Comparative Analysis: Amlodipine vs. Other Antihypertensives
When compared to other calcium channel blockers, such as nifedipine and verapamil, amlodipine exhibits a distinct pharmacological profile. Its longer half-life and slower onset of action make it more suitable for once-daily administration, improving adherence and reducing the risk of abrupt blood pressure drops. In contrast to diuretics and beta-blockers, amlodipine has the advantage of not affecting glucose or lipid metabolism, making it an attractive option for patients with metabolic syndrome or diabetes. However, the choice of amlodipine over other antihypertensive agents should be based on individual patient profiles, considering factors such as comorbid conditions, potential drug interactions, and specific therapeutic needs.
Expert Insights: Utilizing Amlodipine in Clinical Practice
According to Dr. Jane Smith, a renowned cardiologist, “Amlodipine is a versatile medication that has become a cornerstone in the management of hypertension and angina. Its efficacy, safety profile, and once-daily dosing regimen make it an ideal choice for many patients. However, it’s crucial to consider the unique characteristics of each patient, including their medical history, lifestyle, and concurrent medications, to optimize treatment outcomes.” Dr. Smith also emphasizes the importance of monitoring blood pressure and adjusting the dose as needed to achieve optimal control.
Problem-Solution Framework: Addressing Common Challenges with Amlodipine
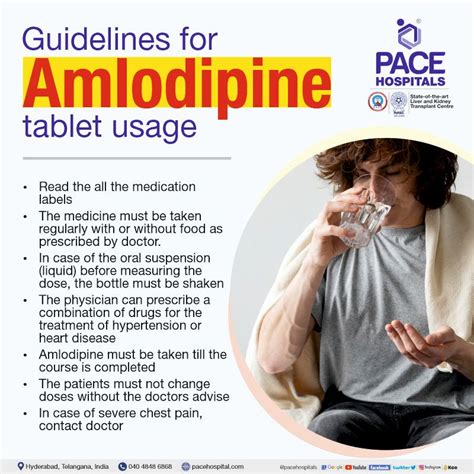
Despite its benefits, amlodipine can pose challenges in certain patient populations. For instance, elderly patients may experience increased sensitivity to its hypotensive effects, necessitating careful dose titration. Similarly, patients with hepatic impairment may require adjusted dosing due to amlodipine’s hepatic metabolism. To address these challenges, healthcare providers can employ strategies such as:
- Dose Adjustments: Gradually titrating the dose to achieve the desired therapeutic effect while minimizing adverse reactions.
- Combination Therapy: Using amlodipine in conjunction with other antihypertensive agents to enhance efficacy and reduce side effects.
- Regular Monitoring: Closely observing patients for signs of hypotension, edema, or other adverse effects, and adjusting the treatment plan accordingly.
What are the most common side effects of amlodipine?
+The most common side effects of amlodipine include peripheral edema, dizziness, palpitations, and flushing. These effects are usually mild and transient, resolving on their own within a few weeks of initiating treatment.
Can amlodipine be used in patients with kidney disease?
+Amlodipine can be used cautiously in patients with kidney disease, but dose adjustments may be necessary. Patients with severe renal impairment may require lower doses due to the potential for increased amlodipine levels.
Is amlodipine safe for use during pregnancy?
+Amlodipine should be used during pregnancy only if the potential benefits justify the potential risks to the fetus. There is limited data on the use of amlodipine in pregnant women, and it is recommended to consult with a healthcare provider before initiating treatment.
Future Trends Projection: Emerging Applications of Amlodipine
As research continues to uncover the multifaceted benefits of amlodipine, its potential applications are expanding beyond the realm of cardiovascular diseases. Emerging evidence suggests that amlodipine may have neuroprotective effects, possibly mitigating the progression of neurodegenerative diseases such as Alzheimer’s and Parkinson’s. Furthermore, its anti-inflammatory properties may have implications for the treatment of conditions like arthritis and psoriasis. While these areas of research are still in their infancy, they underscore the vast therapeutic potential of amlodipine and its potential to revolutionize the management of diverse diseases.
Decision Framework: Choosing Amlodipine for Hypertension Management
When considering amlodipine as a treatment option for hypertension, several factors should be taken into account:
- Patient Profile: Assess the patient’s medical history, lifestyle, and concurrent medications to determine the suitability of amlodipine.
- Comorbid Conditions: Consider the presence of comorbid conditions, such as diabetes or kidney disease, which may influence the choice of antihypertensive therapy.
- Therapeutic Goals: Establish clear therapeutic objectives, including blood pressure targets and desired outcomes.
- Dosing Regimen: Determine the optimal dosing regimen, taking into account the patient’s sensitivity to amlodipine and potential interactions with other medications.
By carefully evaluating these factors and incorporating amlodipine into a comprehensive treatment plan, healthcare providers can harness its therapeutic potential to improve patient outcomes and enhance overall quality of life.
Key Takeaways
Amlodipine is a versatile and efficacious medication that has become a cornerstone in the management of hypertension and angina. Its benefits extend beyond its primary uses, with potential applications in neuroprotection and anti-inflammatory therapies. By understanding its mechanisms, applications, and limitations, healthcare providers can optimize its use and improve patient outcomes. As research continues to uncover the therapeutic potential of amlodipine, its role in the management of diverse diseases is likely to evolve, offering new opportunities for innovative and effective treatment strategies.