Atrial Fibrillation Cardioversion
Atrial fibrillation, often referred to as AFib, is a common type of arrhythmia characterized by an irregular and often rapid heart rate. This condition occurs when the upper chambers of the heart, known as the atria, beat chaotically and irregularly, out of coordination with the lower chambers of the heart, known as the ventricles. The irregular heartbeat can lead to symptoms such as palpitations, shortness of breath, and fatigue, significantly impacting a person’s quality of life. One of the treatments for atrial fibrillation is cardioversion, a procedure aimed at restoring a normal heart rhythm.
Understanding Atrial Fibrillation
Before diving into the specifics of cardioversion, it’s essential to understand the underlying causes and effects of atrial fibrillation. AFib can be caused by various factors, including high blood pressure, heart valve problems, congenital heart defects, and other heart conditions. The condition can also be triggered by stress, certain medications, and stimulants. In some cases, the cause of AFib may not be identified, which is referred to as lone atrial fibrillation.
Atrial fibrillation not only affects the heart’s efficiency in pumping blood but also increases the risk of blood clots forming in the heart, which can lead to a stroke. Therefore, managing AFib involves not just restoring a regular heart rhythm but also preventing these potential complications.
What is Cardioversion?
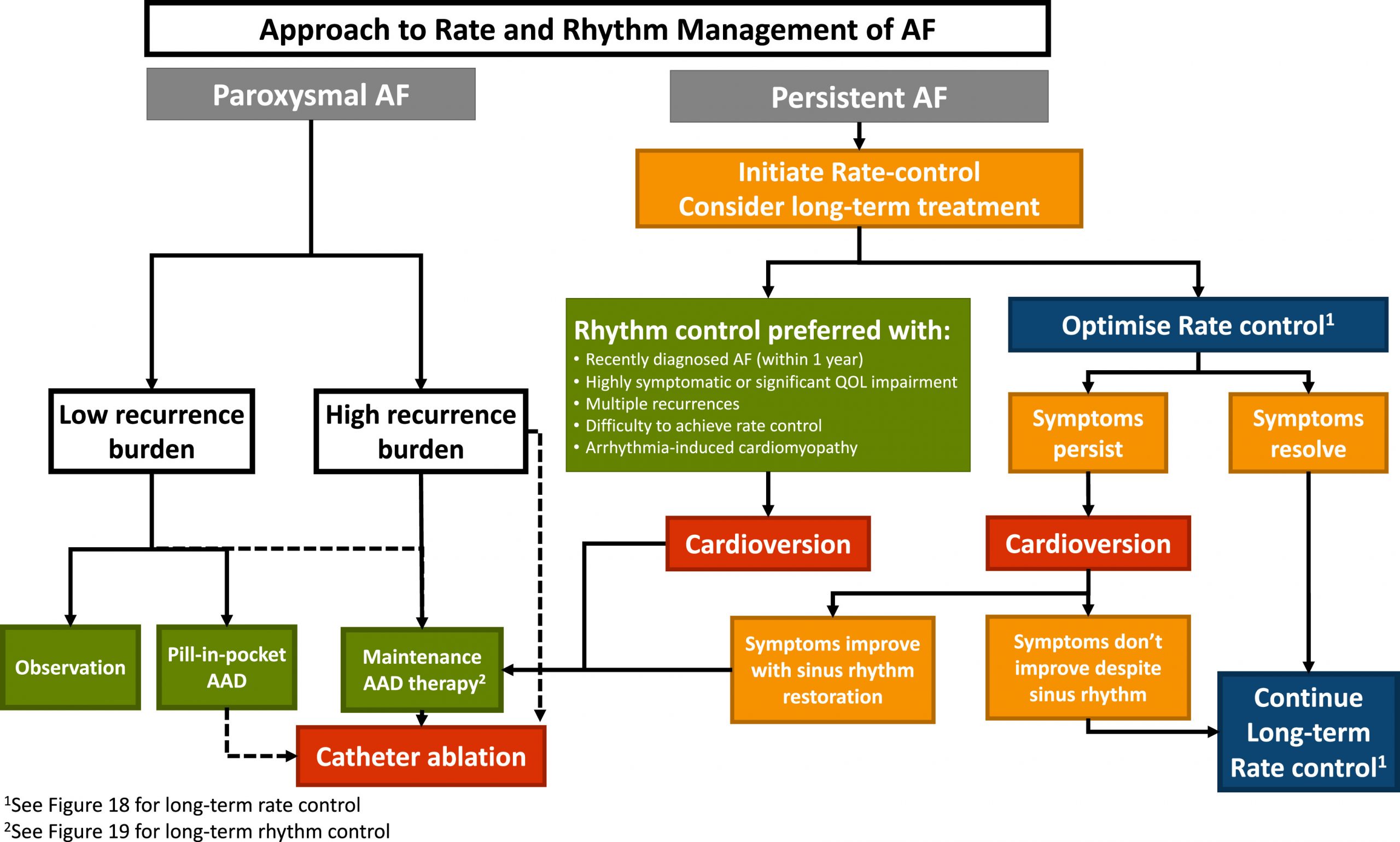
Cardioversion is a medical procedure used to convert an abnormal heart rhythm (arrhythmia) back to a normal rhythm (sinus rhythm) using electrical shocks or medications. In the context of atrial fibrillation, cardioversion is considered when the arrhythmia is symptomatic and other treatments have failed to provide relief or are not suitable.
The procedure can be performed in two main ways:
Electrical Cardioversion: This involves delivering a controlled electric shock to the heart through electrodes placed on the chest. The shock is timed to coincide with the heartbeat and aims to reset the heart’s rhythm. Electrical cardioversion is usually performed under sedation or light anesthesia to minimize discomfort.
Pharmacological Cardioversion: This method uses anti-arrhythmic medications to convert the abnormal heart rhythm back to normal. The choice of medication depends on the patient’s specific condition and medical history. Pharmacological cardioversion is typically attempted before electrical cardioversion, especially in patients with recent-onset AFib.
Preparing for Cardioversion
Before undergoing cardioversion, patients typically undergo a series of tests and evaluations to ensure they are suitable candidates for the procedure. These may include:
- Electrocardiogram (ECG or EKG): To confirm the presence of atrial fibrillation.
- Echocardiogram: To visualize the heart and check for any blood clots in the atria.
- Blood Tests: To assess the patient’s blood clotting factors and rule out other conditions.
- Transesophageal Echocardiogram (TEE): May be required to check for blood clots in the atria, especially if the patient has been in AFib for an extended period or if the risk of clot formation is high.
Patients are also advised to stop taking any anti-arrhythmic medications for a specified period before the procedure and to fast for a certain duration if sedation is planned.
Risks and Complications
While cardioversion is generally a safe procedure, there are potential risks and complications, including:
- Blood Clots and Stroke: The risk of blood clots forming and potentially leading to a stroke is higher after cardioversion, especially if the patient has not been adequately anticoagulated beforehand.
- Cardiac Tamponade: Bleeding into the space surrounding the heart, which can compress the heart and impede its function.
- Pulmonary Edema: Fluid accumulation in the lungs, which can lead to breathing difficulties.
- Reaction to Sedation: Some patients may experience adverse reactions to the sedation used during electrical cardioversion.
After the Procedure
Following cardioversion, patients are typically monitored for a period in a recovery area to ensure the heart rhythm has converted successfully and to watch for any immediate complications. It’s common for patients to feel tired and experience some discomfort or skin irritation at the site where the electrodes were placed.
Patients are usually advised to:
- Avoid Strenuous Activities: For a few days after the procedure to minimize the risk of complications.
- Take Medications as Prescribed: Including anticoagulants to prevent blood clot formation and anti-arrhythmic medications to maintain a normal heart rhythm.
- Follow Up with Their Healthcare Provider: To check on the heart rhythm and adjust medications as necessary.
Long-Term Outlook
The success of cardioversion in restoring and maintaining a normal heart rhythm varies among individuals. Some people may experience a recurrence of atrial fibrillation over time, which may require additional treatments, including repeated cardioversions, medication adjustments, or other interventions like catheter ablation.
FAQs
What are the chances of cardioversion being successful?
+The success of cardioversion depends on various factors, including how long the patient has had atrial fibrillation, the underlying heart health, and the presence of other medical conditions. Generally, the sooner cardioversion is performed after the onset of AFib, the higher the success rate.
How long does it take to recover from cardioversion?
+Most people can resume their normal activities within a few days after the procedure. However, it's essential to follow the specific recovery instructions provided by the healthcare team to minimize the risk of complications.
Can cardioversion be performed more than once if AFib recurs?
+Conclusion
Atrial fibrillation cardioversion offers a potentially effective treatment for restoring a normal heart rhythm in individuals with symptomatic AFib. While it’s crucial to understand the procedure’s benefits and risks, it’s also important to consider it as part of a comprehensive management plan that addresses the underlying causes of AFib, prevents complications, and improves the patient’s quality of life. By working closely with healthcare providers, individuals can make informed decisions about their treatment and take proactive steps towards managing their condition effectively.