Bilirubin Direct Bilirubin
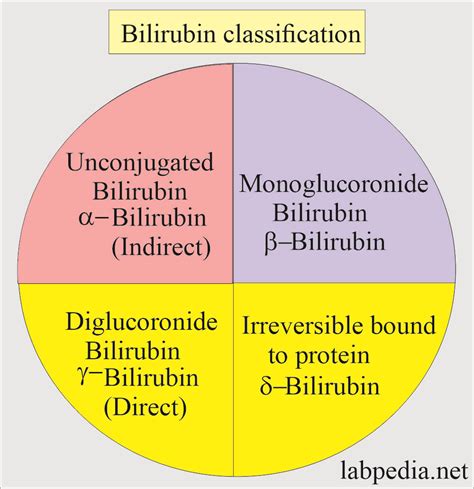
Bilirubin is a yellow compound that occurs in the normal catabolic pathway that breaks down heme in red blood cells. The level of bilirubin in the blood is an important indicator of liver function and can be used to diagnose and monitor various liver disorders. There are two main types of bilirubin: indirect (unconjugated) bilirubin and direct (conjugated) bilirubin.
What is Direct Bilirubin?
Direct bilirubin, also known as conjugated bilirubin, is a type of bilirubin that has been processed by the liver and is now water-soluble. This process, called conjugation, involves the attachment of glucuronic acid to the bilirubin molecule, making it more soluble in water. Direct bilirubin is then excreted into the bile and eventually into the intestines, where it is converted into urobilinogen and excreted in the stool.
Comparison of Indirect and Direct Bilirubin
| Indirect Bilirubin | Direct Bilirubin | |
|---|---|---|
| Solubility | Insoluble in water | Soluble in water |
| Conjugation | Unconjugated | Conjugated |
| Location | Found in blood, not excreted in bile | Excreted in bile, found in stool |
| Clinical Significance | Elevated in hemolytic anemias | Elevated in liver diseases, biliary obstruction |
Elevated Direct Bilirubin: Causes and Clinical Significance
An elevated level of direct bilirubin in the blood can indicate a problem with the liver or bile ducts. Some common causes of elevated direct bilirubin include:
- Liver diseases: Hepatitis, cirrhosis, and liver cancer can all cause an increase in direct bilirubin levels.
- Biliary obstruction: Blockage of the bile ducts, such as by a gallstone or tumor, can prevent direct bilirubin from being excreted into the intestines, leading to a buildup in the blood.
- Cholestasis: A condition in which bile flow is reduced or blocked, leading to a buildup of direct bilirubin in the blood.
Clinical Implications of Elevated Direct Bilirubin
Elevated direct bilirubin levels can have significant clinical implications, including:
- Jaundice: A yellowing of the skin and eyes, which can be a symptom of liver disease or biliary obstruction.
- Pruritus: Itching of the skin, which can be a symptom of cholestasis.
- Fatigue: A feeling of tiredness or weakness, which can be a symptom of liver disease.
- Abdominal pain: Pain in the abdomen, which can be a symptom of liver disease or biliary obstruction.
Diagnostic Approach
A diagnostic approach to elevated direct bilirubin levels may include:
- Complete blood count (CBC): To rule out hemolytic anemia.
- Liver function tests (LFTs): To assess liver damage or dysfunction.
- Imaging studies: Such as ultrasound or CT scan, to visualize the liver and bile ducts.
- Endoscopic retrograde cholangiopancreatography (ERCP): To visualize the bile ducts and diagnose biliary obstruction.
Treatment and Management
Treatment and management of elevated direct bilirubin levels depend on the underlying cause. Some possible treatments include:
- Medications: To manage symptoms such as pruritus and fatigue.
- Surgery: To relieve biliary obstruction or remove a tumor.
- Liver transplantation: In cases of end-stage liver disease.
What is the normal range for direct bilirubin levels in the blood?
+The normal range for direct bilirubin levels in the blood is typically less than 0.3 mg/dL.
What are the symptoms of elevated direct bilirubin levels?
+Symptoms of elevated direct bilirubin levels can include jaundice, pruritus, fatigue, and abdominal pain.
How is elevated direct bilirubin diagnosed and managed?
+Elevated direct bilirubin is diagnosed through a combination of physical examination, laboratory tests, and imaging studies. Management depends on the underlying cause and may include medications, surgery, or liver transplantation.
In conclusion, direct bilirubin is an important indicator of liver function and can be used to diagnose and monitor various liver disorders. Elevated levels of direct bilirubin can have significant clinical implications, and a diagnostic approach should include a combination of laboratory tests, imaging studies, and physical examination. Treatment and management depend on the underlying cause and may include medications, surgery, or liver transplantation.