Bladder Sling Procedure
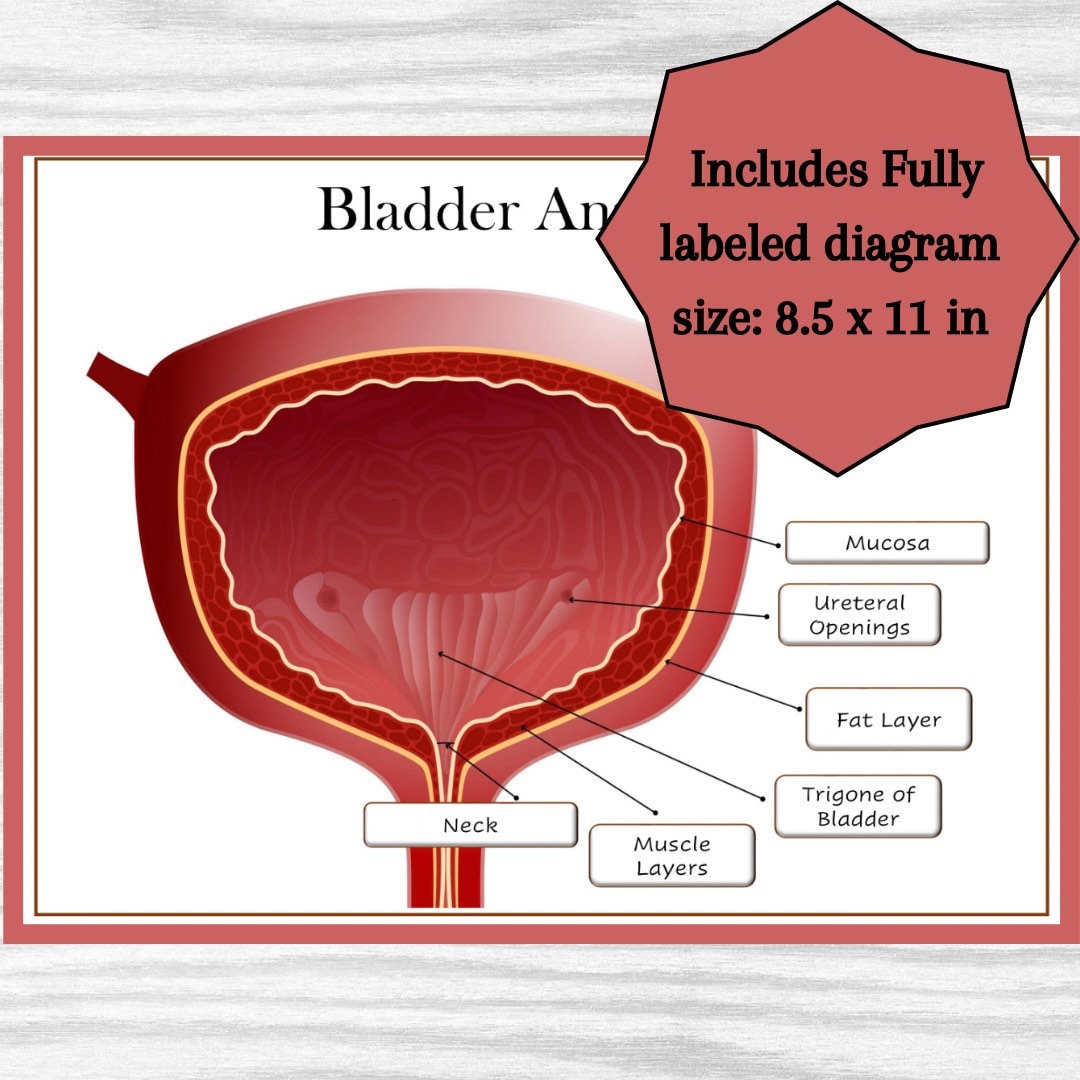
The bladder sling procedure is a surgical intervention designed to treat urinary incontinence, particularly stress urinary incontinence (SUI), in women. This condition occurs when physical movement or pressure (such as coughing, sneezing, laughing, or exercise) causes involuntary leakage of urine. The procedure involves the placement of a sling or hammock under the urethra to provide support and prevent leakage.
Understanding Stress Urinary Incontinence (SUI)
Stress urinary incontinence is a common condition that affects many women, often as a result of childbirth, pregnancy, or menopause, which can weaken the muscles that support the bladder and urethra. When these muscles are weakened, they can no longer provide the necessary support to the urethra, leading to involuntary urine leakage during physical activities. The bladder sling procedure is one of the surgical options available to treat SUI, offering a minimally invasive solution with a high success rate.
How the Bladder Sling Procedure Works
The bladder sling procedure typically involves the following steps:
- Preparation: The patient is given general or local anesthesia to ensure comfort during the procedure. The choice of anesthesia depends on the patient’s health and the surgeon’s preference.
- Incision and Dissection: A small incision is made in the vagina, and the surgeon carefully dissects the tissue to locate the urethra.
- Sling Placement: A sling, made from biological or synthetic material, is then placed under the urethra. This sling acts as a supportive hammock, keeping the urethra in its correct position and preventing urine leakage.
- Adjustment and Securing: The sling is adjusted to provide the right amount of support without constricting the urethra. It is then secured in place with sutures or other fixation methods.
- Closure: The incision is closed, and the procedure is completed.
Types of Slings Used
There are various types of slings used in the bladder sling procedure, including:
- Biological Slings: These are made from natural tissues, such as fascia (a type of connective tissue), and are often harvested from the patient’s own body or from a donor.
- Synthetic Slings: Made from man-made materials like polypropylene, these slings are durable and have been used successfully in many patients.
Benefits of the Bladder Sling Procedure
The bladder sling procedure offers several benefits, including:
- High Success Rate: Many women experience significant improvement or complete resolution of their SUI symptoms after the procedure.
- Minimally Invasive: The procedure involves small incisions, leading to less tissue damage, reduced risk of complications, and quicker recovery times compared to more invasive surgical options.
- Versatility: The procedure can be tailored to the individual’s needs, with various types of slings available to suit different patient requirements.
Risks and Complications
While the bladder sling procedure is generally safe, as with any surgical intervention, there are potential risks and complications, including:
- Infection: As with any surgery, there is a risk of infection.
- Bleeding or Hematoma: Excessive bleeding or the formation of a hematoma (a collection of blood outside of blood cells) can occur.
- Urinary Retention: Some women may experience difficulty emptying their bladder after the procedure.
- Erosion of the Sling: In some cases, the sling material can erode through the urethra or vagina, requiring additional surgery.
Recovery and Post-Operative Care
Recovery from the bladder sling procedure typically involves:
- Rest: Patients are advised to rest and avoid strenuous activities for several weeks after the procedure.
- Pain Management: Managing pain is crucial in the post-operative period, and patients are usually prescribed pain medication.
- Follow-Up Appointments: Regular follow-up appointments with the surgeon are essential to monitor healing and address any concerns or complications.
- Pelvic Floor Exercises: Patients are often encouraged to perform pelvic floor (Kegel) exercises to strengthen the muscles that support the bladder and urethra.
Alternatives to the Bladder Sling Procedure
For women who are not good candidates for the bladder sling procedure or who prefer not to undergo surgery, there are alternative treatments available, including:
- Pelvic Floor Therapy: Physical therapy that focuses on strengthening the pelvic floor muscles.
- Urethral Injectables: Materials injected into the urethral sphincter to improve its closure and prevent leakage.
- Pessaries: Devices inserted into the vagina to provide support to the bladder and urethra.
Conclusion
The bladder sling procedure is an effective surgical option for treating stress urinary incontinence in women. With its high success rate, minimal invasiveness, and adaptability to individual patient needs, it has become a preferred choice for many suffering from SUI. However, as with any medical procedure, it’s essential to weigh the benefits against the potential risks and to discuss all options thoroughly with a healthcare provider to make an informed decision.
What is the success rate of the bladder sling procedure?
+The bladder sling procedure has a high success rate, with many women experiencing significant improvement or complete resolution of their stress urinary incontinence symptoms. Success rates can vary depending on the type of sling used and individual patient factors, but overall, it is considered an effective treatment option.
How long does it take to recover from the bladder sling procedure?
+Recovery time from the bladder sling procedure can vary, but most women can return to their normal activities within a few weeks. It’s generally recommended to avoid strenuous activities, heavy lifting, and intercourse for 4-6 weeks after the procedure to allow for proper healing.
Are there any alternatives to the bladder sling procedure for treating stress urinary incontinence?
+Yes, there are alternative treatments for stress urinary incontinence, including pelvic floor therapy, urethral injectables, and pessaries. The choice of treatment depends on the severity of the condition, the patient’s overall health, and personal preferences. It’s important to discuss all options with a healthcare provider to determine the best course of treatment.