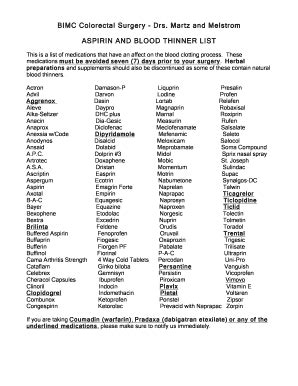
Blood Thinners List
Blood thinners, also known as anticoagulants, are medications that prevent blood clots from forming or growing. They are often prescribed for individuals at risk of developing conditions such as deep vein thrombosis, pulmonary embolism, atrial fibrillation, and stroke. The primary goal of blood thinners is to reduce the risk of these potentially life-threatening conditions by preventing the formation of blood clots.
There are several types of blood thinners available, each with its own unique mechanism of action, benefits, and risks. Here’s a comprehensive list of commonly used blood thinners, categorized by their classification:
1. Warfarin (Coumadin)
- Class: Vitamin K antagonist
- Use: Primarily used for long-term prevention of thromboembolic events in patients with atrial fibrillation, mechanical heart valves, and those at risk for recurrent deep vein thrombosis and pulmonary embolism.
- Monitoring: Requires regular blood tests (INR) to ensure the blood is thinned to the correct degree.
2. Aspirin (Acetylsalicylic Acid)
- Class: Antiplatelet agent
- Use: Often used in low doses to prevent heart attacks and strokes in patients with cardiovascular disease. It works by preventing platelets from clumping together to form blood clots.
- Note: While aspirin has some blood-thinning effects, it’s not as potent as anticoagulants and is generally used for different conditions.
3. Clopidogrel (Plavix)
- Class: Antiplatelet agent
- Use: Used to prevent blood clots in patients with recent heart attack, stroke, or peripheral artery disease. It works by blocking platelet activation.
- Monitoring: Less monitoring is required compared to warfarin, but it’s essential to follow the prescribed regimen.
4. Prasugrel (Effient)
- Class: Antiplatelet agent
- Use: Similar to clopidogrel but is used for patients undergoing angioplasty. It has a quicker onset of action and may be used in cases where clopidogrel is not effective or appropriate.
- Note: It should be used with caution in patients at higher risk of bleeding.
5. Ticagrelor (Brilinta)
- Class: Antiplatelet agent
- Use: Used to prevent thrombotic events in patients with acute coronary syndrome or those undergoing stent placement. It offers benefits similar to prasugrel but with different side effect profiles.
- Monitoring: Patients should be monitored for any signs of bleeding.
6. Dabigatran (Pradaxa)
- Class: Direct oral anticoagulant (DOAC)
- Use: Used for stroke prevention in atrial fibrillation not caused by heart valve problems, as well as for the treatment and prevention of deep vein thrombosis and pulmonary embolism.
- Note: It’s a more convenient option than warfarin because it doesn’t require regular blood tests, but it has a higher risk of gastrointestinal bleeding.
7. Rivaroxaban (Xarelto)
- Class: DOAC
- Use: Indicated for stroke prevention in non-valvular atrial fibrillation, treatment and prevention of deep vein thrombosis and pulmonary embolism, and for reducing the risk of recurrent events in patients with acute coronary syndrome.
- Monitoring: Like dabigatran, it offers a fixed dosing regimen without the need for regular blood monitoring.
8. Apixaban (Eliquis)
- Class: DOAC
- Use: Similar to rivaroxaban, used for stroke prevention in atrial fibrillation, treatment of deep vein thrombosis and pulmonary embolism, and for reducing the risk of recurrent events in patients with acute coronary syndrome.
- Note: Clinical trials have shown a lower risk of bleeding compared to warfarin.
9. Edoxaban (Savaysa, Lixiana)
- Class: DOAC
- Use: Used for preventing stroke and systemic embolism in patients with non-valvular atrial fibrillation and for treating deep vein thrombosis and pulmonary embolism.
- Monitoring: Offers once or twice daily dosing options with reduced risk of bleeding in certain patient populations.
Important Considerations
- Bleeding Risk: All blood thinners increase the risk of bleeding. The risk varies among medications, and the decision to start a blood thinner involves weighing this risk against the benefits of preventing blood clots.
- Interactions: Many medications, including over-the-counter drugs and supplements, can interact with blood thinners, either increasing the risk of bleeding or reducing their effectiveness.
- Lifestyle Adjustments: Patients on blood thinners may need to make lifestyle adjustments, such as avoiding certain foods (for warfarin), limiting alcohol intake, and being cautious during activities that could lead to injury.
Each blood thinner has its unique benefits and risks, and the choice of which one to use depends on the individual’s health condition, the presence of other medical conditions, and the potential for drug interactions. It’s crucial for patients to follow their healthcare provider’s instructions carefully and attend all scheduled follow-up appointments to monitor the effectiveness and safety of their blood thinner regimen.
What are the main differences between antiplatelet agents and anticoagulants?
+Antiplatelet agents (like aspirin and clopidogrel) prevent platelets from clumping together to form a blood clot, whereas anticoagulants (like warfarin and the DOACs) work by interfering with the blood clotting process itself, usually by inhibiting the production of vitamin K-dependent clotting factors or directly inhibiting thrombin or factor Xa. This fundamental difference affects how and when they are used in clinical practice.
How do DOACs compare to warfarin in terms of convenience and efficacy?
+DOACs offer several advantages over warfarin, including a fixed dosing regimen, fewer dietary restrictions, and no need for regular blood monitoring (INR checks). Clinical trials have shown that DOACs are at least as effective as warfarin in preventing stroke in patients with atrial fibrillation and have a more predictable pharmacokinetic profile, which reduces the risk of drug interactions. However, the choice between DOACs and warfarin depends on individual patient factors, including cost, the presence of kidney disease, and personal preference.
What should patients do if they miss a dose of their blood thinner?
+If a patient misses a dose of their blood thinner, they should contact their healthcare provider for advice. The action to take depends on the specific medication and how long it has been since the missed dose. For some medications, taking the missed dose as soon as remembered is appropriate, while for others, doubling up on the next dose is not recommended due to an increased risk of bleeding. It’s crucial not to make these decisions without consulting a healthcare professional.