Bronchitis Antibiotics Guide: Know When
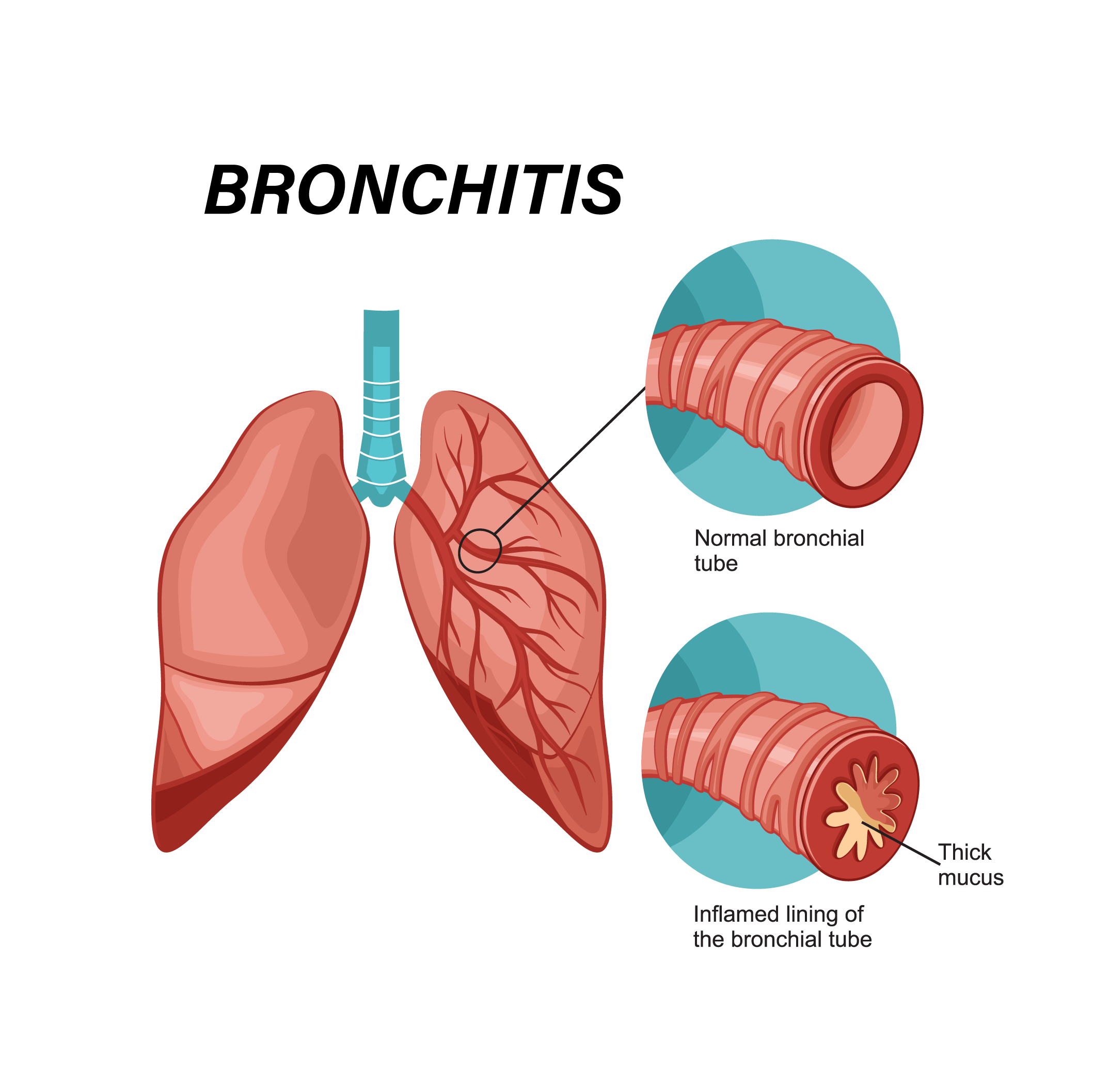
Bronchitis, a common respiratory condition characterized by inflammation of the bronchial tubes, can be a debilitating and frustrating experience for those affected. The decision to use antibiotics in treating bronchitis is a critical one, given the potential for misuse and the rise of antibiotic-resistant bacteria. Understanding when antibiotics are necessary and when they might not be the best course of action is essential for both healthcare providers and patients. This guide aims to provide a comprehensive overview of the role of antibiotics in bronchitis treatment, helping to clarify the nuances of their use in this context.
Understanding Bronchitis
Before delving into the specifics of antibiotic treatment, it’s crucial to understand the basics of bronchitis. Bronchitis can be acute or chronic. Acute bronchitis is a short-term inflammation of the bronchial tubes, often resulting from a viral infection, although it can also be caused by bacterial infections or exposure to irritants like smoke or dust. Chronic bronchitis, on the other hand, is a long-standing inflammation of the bronchial tubes, predominantly associated with smoking but also with prolonged exposure to air pollutants.
The Role of Antibiotics in Bronchitis Treatment
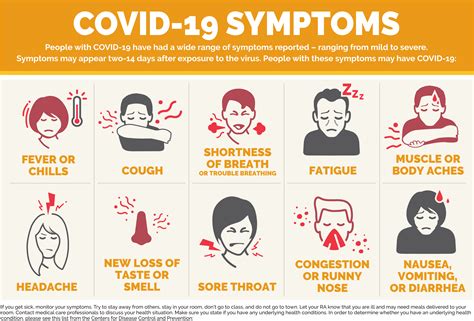
Antibiotics are effective against bacterial infections but not against viral infections. The majority of acute bronchitis cases are caused by viruses, which means that antibiotics would not be beneficial in these instances. However, distinguishing between viral and bacterial bronchitis can be challenging, as the symptoms often overlap.
Identifying Bacterial Bronchitis
Healthcare providers use various criteria to determine if bronchitis might be bacterial, including the presence of certain symptoms, the duration of the illness, and the patient’s overall health status. Specific signs that might indicate a bacterial infection include:
- Prolonged Symptoms: If symptoms persist or worsen over time, particularly if coughing persists for more than two weeks.
- High Fever: The presence of a high fever, often above 102°F (39°C), can be indicative of a bacterial infection.
- Difficulty Breathing: Severe difficulty breathing or shortness of breath.
- Discolored Mucus: Coughing up discolored or bloody mucus can sometimes indicate a bacterial infection.
Antibiotic Use in Chronic Bronchitis
In the case of chronic bronchitis, which is often a component of chronic obstructive pulmonary disease (COPD), the role of antibiotics can be more complex. While antibiotics are not used to treat the underlying condition, they may be prescribed during acute exacerbations of chronic bronchitis (AECB) if a bacterial infection is suspected. The decision to use antibiotics in AECB is guided by the severity of symptoms, the presence of discharge, and changes in the color or volume of sputum.
Risks and Considerations of Antibiotic Use
While antibiotics can be life-saving in cases of bacterial infections, their misuse or overuse can lead to significant risks, including:
- Antibiotic Resistance: The development of bacteria that are resistant to antibiotics, making infections harder to treat.
- Side Effects: Antibiotics can cause a range of side effects, from mild to severe, including allergic reactions, diarrhea, and yeast infections.
- Disruption of Gut Flora: Antibiotics can alter the balance of gut bacteria, potentially leading to other health issues.
Alternatives and Complementary Treatments
For viral bronchitis or cases where antibiotics are not indicated, several alternatives and complementary treatments can help manage symptoms and support recovery:
- Rest and Hydration: Getting plenty of rest and staying hydrated can help the body recover from illness.
- Over-the-Counter Medications: Cough suppressants, expectorants, and pain relievers can help manage cough, congestion, and discomfort.
- Humidifiers: Adding moisture to the air can help soothe a sore throat and reduce coughing.
- Saline Nasal Sprays: Can help moisturize the nasal passages and thin out mucus, making it easier to expel.
Future Directions and Current Research
Research continues into the causes and treatments of bronchitis, including the development of new antibiotics and the exploration of non-antibiotic treatments for bacterial infections. Additionally, there is a growing focus on preventive measures, such as vaccinations against common viral and bacterial pathogens, and public health initiatives to reduce air pollution and promote smoking cessation.
Conclusion
The decision to use antibiotics in treating bronchitis should be made thoughtfully, considering both the potential benefits and the risks. By understanding the differences between viral and bacterial bronchitis and the role of antibiotics in each, patients and healthcare providers can make informed decisions that promote effective treatment while minimizing the misuse of these critical medications.
What is the primary cause of acute bronchitis?
+Acute bronchitis is primarily caused by viral infections, although it can also result from bacterial infections or exposure to irritants.
How can you differentiate between viral and bacterial bronchitis?
+Differentiation can be challenging, but signs of bacterial bronchitis may include prolonged symptoms, high fever, difficulty breathing, and discolored mucus. A healthcare provider’s diagnosis is crucial for determining the cause and appropriate treatment.
What are the risks associated with the overuse of antibiotics in bronchitis treatment?
+The overuse of antibiotics can lead to antibiotic resistance, making infections harder to treat, as well as side effects and disruption of gut flora. It’s essential to use antibiotics judiciously and only when necessary.
What alternative treatments can help manage bronchitis symptoms when antibiotics are not indicated?
+Alternatives include rest, hydration, over-the-counter medications for symptom relief, humidifiers, and saline nasal sprays. These can help manage symptoms and support recovery in cases of viral bronchitis or when antibiotics are not prescribed.
Why is it crucial to differentiate between acute and chronic bronchitis when considering treatment options?
+Acute and chronic bronchitis have different underlying causes and treatment approaches. Chronic bronchitis, often part of COPD, may involve managing symptoms and preventing exacerbations, whereas acute bronchitis treatment focuses on relieving symptoms and addressing the underlying infection, if bacterial.