C Diff Diagnosis: Comprehensive Testing Guide
The diagnosis of Clostridioides difficile (C. diff) infection is a complex process that requires a combination of clinical evaluation, laboratory testing, and sometimes, imaging studies. C. diff is a type of bacteria that can cause symptoms ranging from mild diarrhea to life-threatening colitis. The rise of antibiotic-resistant C. diff strains has made accurate and timely diagnosis crucial for effective treatment and prevention of transmission.
Understanding C. Diff Infection
C. diff infection typically occurs after the use of broad-spectrum antibiotics, which can disrupt the normal balance of gut flora, allowing C. diff to overgrow and produce toxins. The primary symptoms of C. diff infection include watery diarrhea, abdominal cramping, fever, and loss of appetite. In severe cases, it can lead to pseudomembranous colitis, a condition characterized by inflammation of the colon and the formation of a pseudomembrane, a visible layer of inflammatory debris and bacteria.
Clinical Evaluation
The clinical evaluation of a patient suspected of having C. diff infection involves a thorough medical history, physical examination, and review of symptoms. Healthcare providers look for recent antibiotic use, the presence of diarrhea (defined as three or more unformed stools in 24 hours), and other symptoms such as fever, abdominal pain, and weight loss. The clinical evaluation is critical because it guides the decision to perform diagnostic tests and start empiric treatment in severe cases.
Laboratory Testing
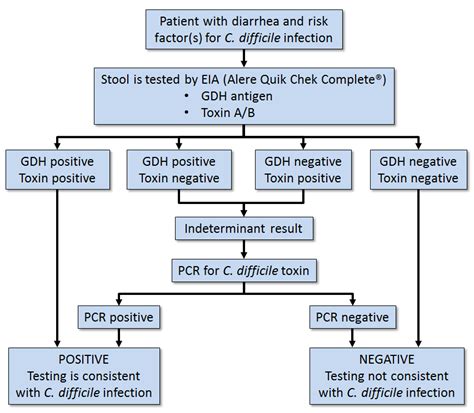
Several laboratory tests can diagnose C. diff infection, each with its own strengths and limitations. The choice of test depends on various factors, including the clinical presentation, availability of testing methods, and institutional protocols.
- Enzyme Immunoassay (EIA) for Toxins: This test detects the presence of C. diff toxins A and B in stool. While it is relatively quick and easy to perform, it has lower sensitivity compared to other methods, which can lead to false-negative results.
- Polymerase Chain Reaction (PCR) for Toxin-Producing C. diff: PCR is a molecular test that detects the genes responsible for toxin production. It is highly sensitive and can identify the presence of toxin-producing C. diff, but it does not distinguish between symptomatic infection and asymptomatic colonization.
- Stool Culture: This involves growing C. diff from a stool sample. Although it can detect the presence of the bacteria, it does not differentiate between toxigenic and non-toxigenic strains, and results can take several days.
- Cell Cytotoxicity Assay: This older method involves assessing the cytotoxic effect of C. diff toxins on cultured cells. While highly specific, it is labor-intensive, takes longer to yield results, and has largely been replaced by PCR and EIA in many laboratories.
Imaging Studies
In some cases, especially when the diagnosis is uncertain or when complications are suspected, imaging studies such as abdominal X-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI) may be performed. These studies can help identify complications of C. diff infection, such as toxic megacolon, bowel obstruction, or perforation, which require immediate medical intervention.
Current Guidelines and Recommendations
Current guidelines recommend a multi-step approach for the diagnosis of C. diff infection, starting with a clinical diagnosis based on symptoms, followed by laboratory confirmation using a combination of tests. For example, using a PCR test as a stand-alone test or as part of a multi-step algorithm that includes EIA for toxins. Repeat testing during the same episode of diarrhea is generally not recommended unless there is a significant change in the patient’s condition.
Infection Control and Prevention
Given the contagious nature of C. diff, especially in healthcare settings, infection control measures are critical. These include isolation of infected patients, use of personal protective equipment (PPE) by healthcare workers, thorough cleaning and disinfection of the patient’s environment, and proper hand hygiene practices.
Future Perspectives and Challenges
The diagnosis and management of C. diff infection continue to evolve, with ongoing research focused on developing more accurate and rapid diagnostic tests, understanding the role of the gut microbiome, and exploring new therapeutic options, including fecal microbiota transplantation (FMT) for recurrent infections. However, challenges persist, including the emergence of hypervirulent strains, the impact of antibiotic stewardship programs on C. diff incidence, and the need for more effective infection control strategies.
Conclusion
The diagnosis of C. diff infection requires a comprehensive approach, incorporating clinical judgment, laboratory testing, and sometimes, imaging studies. As our understanding of this infection evolves, so do the strategies for its diagnosis, treatment, and prevention. By staying abreast of the latest guidelines and advancements, healthcare providers can improve patient outcomes and reduce the spread of this significant healthcare-associated infection.
What is the most accurate test for diagnosing C. diff infection?
+Polymerase Chain Reaction (PCR) for toxin-producing C. diff is considered highly sensitive and is often used for diagnosing C. diff infection. However, the choice of test may depend on the clinical scenario and institutional protocols.
How can C. diff infection be prevented?
+Prevention of C. diff infection involves careful use of antibiotics, proper hand hygiene, isolation of infected patients, and thorough environmental cleaning. In healthcare settings, adherence to infection control policies is crucial.
What are the symptoms of severe C. diff infection?
+Symptoms of severe C. diff infection include severe diarrhea that can lead to dehydration, abdominal tenderness, fever, and signs of sepsis. In the most severe cases, it can cause pseudomembranous colitis or toxic megacolon, which are medical emergencies.
Can C. diff infection be treated without antibiotics?
+While antibiotics are often necessary to treat C. diff infection, particularly for severe cases or initial episodes, treatments like fecal microbiota transplantation (FMT) are being explored for recurrent infections. Supportive care to manage symptoms and prevent complications is also a critical component of treatment.