Chest Catheter For Dialysis
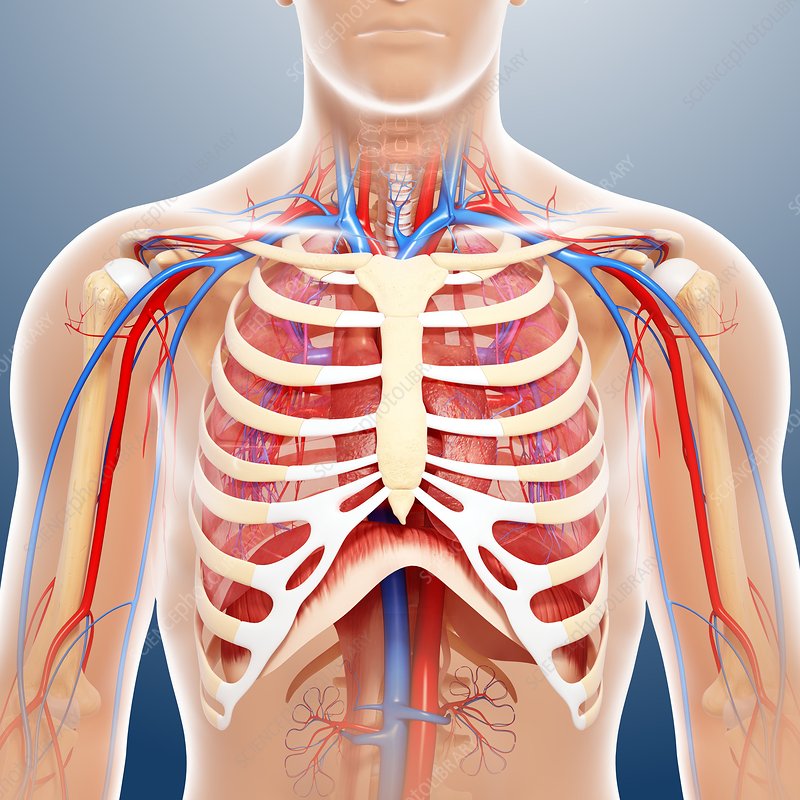
The utilization of chest catheters, also known as central venous catheters, for dialysis has been a crucial component in the management of patients with end-stage renal disease (ESRD). These catheters are inserted into a large vein in the chest, enabling the connection to a dialysis machine for the filtration of waste products from the blood when the kidneys are no longer capable of performing this function. Despite their importance, the use of chest catheters for dialysis is associated with significant risks and complications, making their management and care a complex aspect of patient treatment.
Historical Evolution of Dialysis Access
The history of dialysis access has evolved significantly since the inception of dialysis as a treatment for renal failure. Initially, dialysis was performed using arteriovenous fistulas, which are still considered the gold standard for dialysis access due to their lower risk of infection and thrombosis compared to catheters. However, the development and refinement of central venous catheters have provided a viable alternative for patients who are not candidates for fistula creation or have exhausted other access options.
Technical Breakdown of Chest Catheters
Chest catheters for dialysis are typically made of silicone or polyurethane and consist of two lumens (tubes): one for drawing blood out of the body to the dialysis machine and the other for returning the cleaned blood. The insertion of these catheters involves a minor surgical procedure, often performed under local anesthesia, where the catheter is placed into the superior vena cava via a vein in the neck or chest. The catheter is then secured to the skin with sutures and a dressing to prevent infection and promote healing.
Problem-Solution Framework: Managing Complications
Despite their utility, chest catheters are not without complications. Infection, thrombosis, and catheter malfunction are among the most common issues. To mitigate these risks:
- Infection Control: Strict adherence to sterile technique during insertion and subsequent care, including the use of antimicrobial locks, can significantly reduce the risk of catheter-related bloodstream infections.
- Thrombosis Prevention: The use of anticoagulants and ensuring adequate blood flow through the catheter can help prevent clot formation.
- Catheter Maintenance: Regular flushing of the catheter with heparin or other locking solutions when not in use can prevent occlusion and maintain patency.
Comparative Analysis: Catheters vs. Other Dialysis Access Methods
When comparing chest catheters to arteriovenous fistulas and grafts, several factors come into play:
- Infection Risk: Catheters have a higher risk of infection compared to fistulas and grafts.
- Thrombosis Risk: Similarly, catheters are more prone to thrombosis.
- Patient Satisfaction: Fistulas are often preferred by patients due to their lower complication rate and absence of an external device.
- Lifespan: The lifespan of a catheter is generally shorter than that of a well-crafted fistula or graft.
Expert Insight: Advances in Catheter Technology
Recent advances in catheter technology aim to reduce complications and improve patient outcomes. This includes the development of antimicrobial catheters, improved materials to reduce the risk of thrombosis, and designs that facilitate easier insertion and removal. Furthermore, research into novel locking solutions and anti-infective strategies continues to evolve, promising to enhance the safety and efficacy of chest catheters for dialysis.
Future Trends Projection: Minimally Invasive Techniques
The future of dialysis access is likely to be shaped by advancements in minimally invasive techniques and technologies that reduce the risk of complications associated with traditional catheter placement. Innovations in vascular access creation, such as endovascular approaches, may offer patients safer and more durable options for dialysis.
Decision Framework: Choosing the Right Access for Dialysis
The decision on which type of dialysis access to use is multifaceted and should be tailored to the individual patient’s needs, vascular anatomy, and lifestyle. A comprehensive evaluation considering the patient’s medical history, the presence of suitable veins for fistula creation, and personal preferences is essential. The involvement of a multidisciplinary team, including nephrologists, vascular surgeons, and dialysis nurses, ensures that patients receive the most appropriate and effective dialysis access.
Conclusion
Chest catheters play a vital role in the management of patients undergoing dialysis, offering a lifeline for those with end-stage renal disease. While they are associated with significant risks, continued advancements in technology and care strategies aim to minimize these complications. As the field of nephrology and vascular access continues to evolve, the focus remains on providing patients with the safest, most effective, and patient-centered care possible, tailoring dialysis access to meet the unique needs of each individual.
FAQ Section
What are the primary risks associated with using chest catheters for dialysis?
+The primary risks include infection, thrombosis, and catheter malfunction. Infection control measures and regular catheter maintenance are crucial to mitigating these risks.
How do chest catheters compare to arteriovenous fistulas in terms of complication rates?
+Chest catheters have a higher risk of infection and thrombosis compared to arteriovenous fistulas. Fistulas are generally considered the gold standard for dialysis access due to their lower complication rate and longer lifespan.
What advancements are being made in chest catheter technology to reduce complications?
+Recent advancements include the development of antimicrobial catheters, improved materials to reduce thrombosis risk, and novel designs facilitating easier insertion and removal. Ongoing research into locking solutions and anti-infective strategies also aims to enhance catheter safety and efficacy.