Clindamicina: Effective Acne Treatment Solution

The quest for clear, radiant skin is a universal desire, yet acne remains a pervasive issue affecting millions worldwide. Among the myriad treatments available, clindamycin has emerged as a potent and effective solution for combatting acne. This antibiotic, applied topically or taken orally, has been a cornerstone in dermatological practice for decades, offering hope to those suffering from acne’s physical and emotional scars.
Understanding Acne: The Basis for Effective Treatment
Before delving into the specifics of clindamycin, it’s essential to grasp the underlying causes of acne. Acne vulgaris, the most common form, is characterized by the occurrence of comedones (blackheads and whiteheads), pimples, and sometimes cysts or nodules. The pathogenesis involves a complex interplay of factors including increased sebum production, follicular hyperkeratinization, the presence of Propionibacterium acnes (P. acnes) bacteria, and inflammation.
Clindamycin: Mechanism of Action
Clindamycin belongs to the lincosamide class of antibiotics, which work by inhibiting protein synthesis in bacteria. Specifically, clindamycin binds to the 50S subunit of the bacterial ribosome, thereby preventing the translation of messenger RNA into proteins essential for bacterial growth and replication. In the context of acne, clindamycin targets P. acnes, the bacteria that play a crucial role in the development of inflammatory acne lesions. By reducing the population of P. acnes, clindamycin decreases the production of pro-inflammatory factors, ultimately leading to a reduction in inflammation and acne severity.
Forms and Applications of Clindamycin
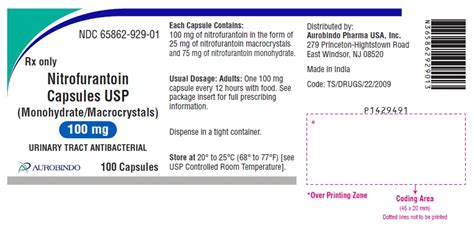
Clindamycin is available in various topical formulations, including gels, lotions, and solutions, as well as oral capsules. The choice between topical and systemic therapy depends on the severity and extent of acne, patient preference, and potential side effects. Topical clindamycin is often preferred for mild to moderate acne due to its localized action and lower risk of systemic side effects. Oral clindamycin is reserved for more severe cases, including acne that is resistant to other treatments or when there is a significant risk of scarring.
Efficacy of Clindamycin in Acne Treatment
Numerous clinical trials and studies have demonstrated the efficacy of clindamycin in reducing acne lesions. When used topically, clindamycin has been shown to significantly decrease the number of inflammatory and non-inflammatory lesions compared to placebo. Furthermore, combination therapy, where clindamycin is used alongside other acne treatments such as benzoyl peroxide or retinoids, can enhance efficacy by targeting multiple pathogenic factors of acne.
Safety and Side Effects
While clindamycin is generally well-tolerated, both topical and oral forms can be associated with side effects. Common adverse effects of topical clindamycin include dryness, redness, and itching at the application site. Systemic use of clindamycin can lead to more serious side effects, including gastrointestinal disturbances, pseudomembranous colitis, and potential interactions with other medications. It is crucial for patients to follow the prescribed regimen and report any concerns or side effects to their healthcare provider.
Clindamycin and Antibiotic Resistance
The increasing prevalence of antibiotic-resistant bacterial strains is a global concern. The use of antibiotics, including clindamycin, for acne treatment has raised concerns about contributing to resistance. However, the development of resistance to clindamycin among P. acnes is relatively rare compared to other antibiotics. Nonetheless, responsible use, including the shortest effective treatment duration and combination with other non-antibiotic treatments, is recommended to mitigate this risk.
Conclusion
Clindamycin represents a valuable option in the treatment arsenal against acne, offering a potent solution for reducing bacterial loads and inflammation. Its efficacy, combined with a generally favorable safety profile, makes it a commonly prescribed medication for patients suffering from acne. As with any treatment, careful consideration of potential side effects, the risk of resistance, and the importance of adherence to the prescribed regimen are paramount. By understanding the mechanism, applications, and limitations of clindamycin, healthcare providers and patients can work together to effectively manage acne and reclaim the confidence that comes with clear, healthy skin.
How does clindamycin work to treat acne?
+Clindamycin works by inhibiting protein synthesis in bacteria, specifically targeting Propionibacterium acnes (P. acnes), which plays a significant role in the development of acne. By reducing the bacterial load, clindamycin decreases inflammation and the severity of acne lesions.
What are the common side effects of using clindamycin for acne treatment?
+Common side effects of topical clindamycin include dryness, redness, and itching at the application site. Systemic use can lead to more serious side effects like gastrointestinal disturbances and potential interactions with other medications. It's essential to follow the prescribed regimen and report any concerns to a healthcare provider.
Can clindamycin be used in combination with other acne treatments?
+Yes, clindamycin is often used in combination with other treatments such as benzoyl peroxide or retinoids. Combination therapy can enhance efficacy by targeting multiple factors that contribute to acne, including bacteria, inflammation, and clogged pores.
In the realm of acne treatment, clindamycin stands as a testament to the advancements in dermatological care, providing a reliable and effective solution for many. As research continues to evolve and new treatments emerge, the strategic use of clindamycin, either alone or in combination with other therapies, will remain a critical component in the quest for acne-free skin.