Cms 1500 Hcfa Claim Forms
The CMS 1500 form, also known as the HCFA 1500 form, is a standard claim form used by healthcare providers to bill Medicare and other health insurance companies for services rendered. The form is designed to capture all the necessary information required for processing claims, including patient demographics, service details, and billing information.
Introduction to the CMS 1500 Form
The CMS 1500 form is a crucial document in the healthcare billing process. It is used by healthcare providers to submit claims to Medicare, Medicaid, and other private insurance companies. The form is designed to be easy to use and understand, with clear instructions and guidelines to ensure accurate completion. The CMS 1500 form is typically completed by the healthcare provider’s billing staff or administrative team, who are responsible for ensuring that all necessary information is accurately captured and submitted to the relevant insurance companies.
Key Components of the CMS 1500 Form
The CMS 1500 form consists of several key components, including:
- Patient Information: This section captures the patient’s demographics, including name, address, date of birth, and insurance information.
- Service Information: This section details the services provided to the patient, including the date of service, procedure codes, and diagnosis codes.
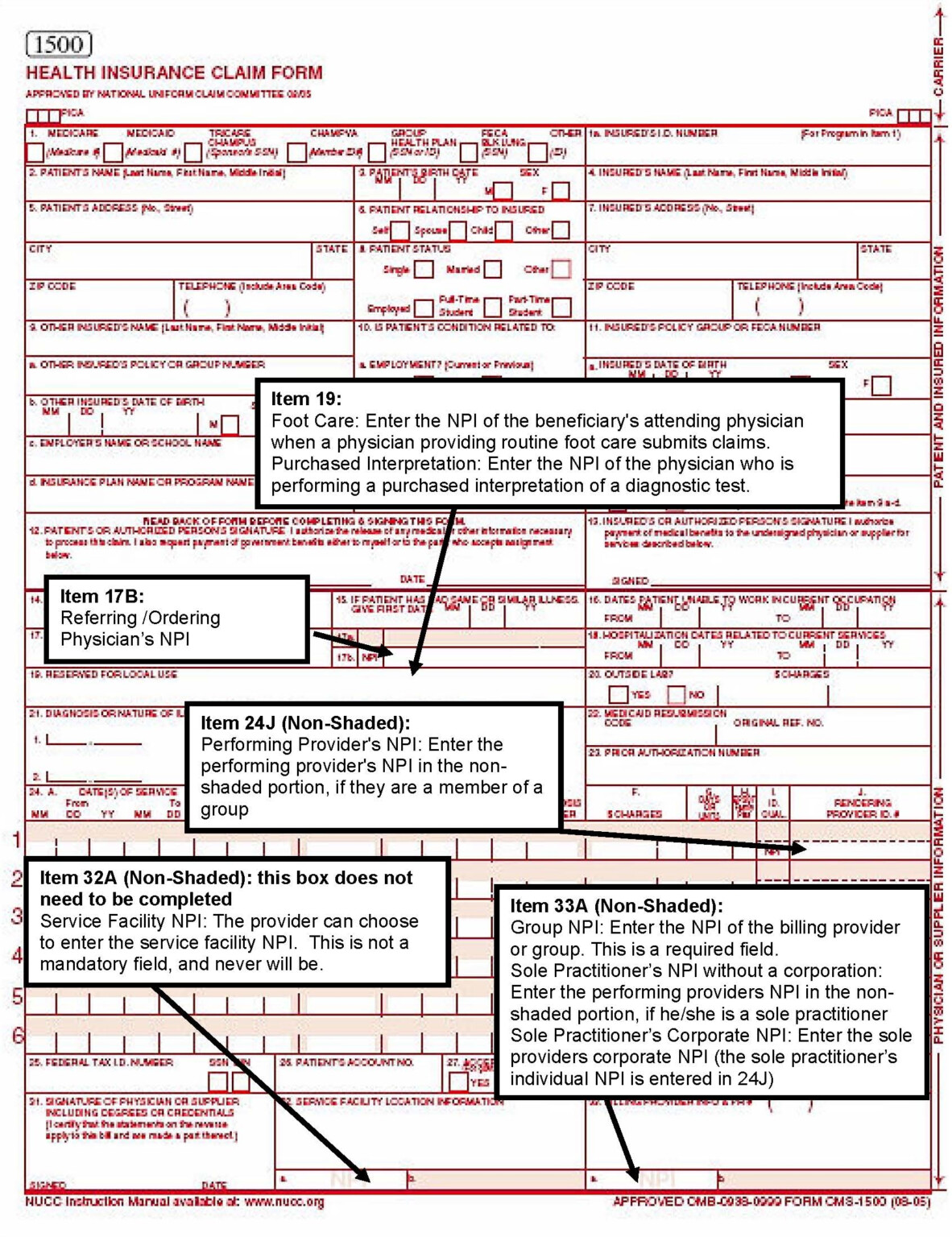
- Billing Information: This section captures the billing information, including the healthcare provider’s name, address, and national provider identifier (NPI) number.
- Charges and Payments: This section details the charges for the services provided, as well as any payments made or due.
Completing the CMS 1500 Form
To complete the CMS 1500 form, healthcare providers must ensure that all necessary information is accurately captured and submitted. Here are some tips to help ensure accurate completion:
- Use clear and concise language: Avoid using abbreviations or codes that may not be easily understood by the insurance company.
- Double-check patient information: Ensure that the patient’s demographics are accurately captured, including name, address, and date of birth.
- Use correct procedure and diagnosis codes: Ensure that the correct procedure codes (e.g., CPT or HCPCS) and diagnosis codes (e.g., ICD-10) are used to describe the services provided.
- Calculate charges accurately: Ensure that charges are accurately calculated and reflect the services provided.
Common Mistakes to Avoid
When completing the CMS 1500 form, there are several common mistakes to avoid, including:
- Inaccurate patient information: Incorrect or incomplete patient information can lead to delays or denials in claim processing.
- Incorrect procedure or diagnosis codes: Using incorrect codes can lead to claim denials or underpayment.
- Inconsistent or missing information: Inconsistent or missing information can lead to delays or denials in claim processing.
Frequently Asked Questions (FAQs)
What is the purpose of the CMS 1500 form?
+The CMS 1500 form is used by healthcare providers to submit claims to Medicare and other health insurance companies for services rendered.
What information is required on the CMS 1500 form?
+The CMS 1500 form requires patient demographics, service details, and billing information, including procedure codes, diagnosis codes, and charges.
How do I avoid common mistakes when completing the CMS 1500 form?
+To avoid common mistakes, ensure that patient information is accurate, procedure and diagnosis codes are correct, and charges are accurately calculated.
Conclusion
The CMS 1500 form is a critical document in the healthcare billing process. By understanding the key components of the form and following tips for accurate completion, healthcare providers can ensure that claims are processed efficiently and accurately. Avoiding common mistakes and using correct procedure and diagnosis codes can help prevent delays or denials in claim processing. By following these guidelines, healthcare providers can streamline their billing process and improve reimbursement rates.



