Cochlear Implant Surgery

The advent of cochlear implant surgery has revolutionized the treatment of severe to profound sensorineural hearing loss, offering a lifeline to individuals who were previously unable to perceive sound. This complex procedure involves the implantation of a sophisticated device that bypasses damaged portions of the ear to directly stimulate the auditory nerve, thereby restoring a sense of hearing.
What is Cochlear Implant Surgery?
Cochlear implant surgery is a meticulous operation that requires precision, expertise, and the latest technology. The procedure involves several key components, including an external sound processor, a transmitter, a receiver/stimulator, and an electrode array. The external sound processor captures sound from the environment, which is then converted into electrical signals and transmitted across the skin to the implanted receiver/stimulator. This device, in turn, sends the signals through the electrode array inserted into the cochlea, the spiral-shaped structure in the inner ear responsible for sound processing. The electrical stimulation of the cochlea directly activates the auditory nerve, allowing the brain to interpret these signals as sound.
Historical Evolution of Cochlear Implants
The concept of cochlear implants has undergone significant evolution since its inception. The first cochlear implant was developed in the 1950s by André Djourno and Charles Eyriès, but these early devices were rudimentary and provided limited benefits. Over the decades, advancements in technology, materials science, and surgical techniques have transformed cochlear implants into the sophisticated devices used today. Modern cochlear implants are capable of processing a wide range of sounds, from simple tones to complex speech and music, significantly improving the quality of life for recipients.
Candidacy and Evaluation
Not everyone with hearing loss is a candidate for cochlear implant surgery. A comprehensive evaluation by an interdisciplinary team, including audiologists, otolaryngologists (ENT surgeons), and speech-language pathologists, is essential to determine candidacy. This process involves a series of tests, including audiological assessments, imaging studies like CT or MRI scans, and psychological evaluations. The primary criteria for candidacy include severe to profound sensorineural hearing loss in one or both ears, limited benefit from traditional hearing aids, and no medical conditions that would pose a risk for the surgery.
Surgical Procedure
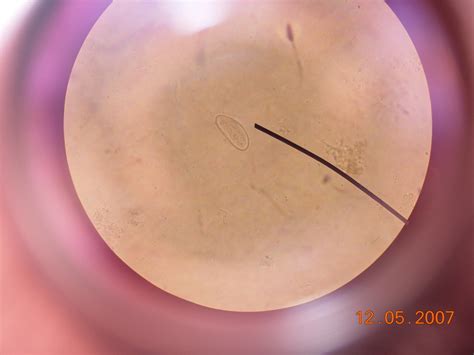
The cochlear implant surgery is typically performed under general anesthesia and can take several hours to complete. The procedure begins with the surgeon making an incision behind the ear to access the Cochlea. A small opening, known as a cochleostomy, is made in the cochlea, and the electrode array is carefully inserted. The receiver/stimulator is then placed under the skin behind the ear, and the incision is closed. Post-operative care includes managing pain and monitoring for any signs of infection or complications.
Recovery and Rehabilitation
Recovery from cochlear implant surgery is usually smooth, with most individuals returning home the same day or the day after surgery. The external sound processor is typically activated about 2-4 weeks after surgery, a process known as “mapping.” This involves an audiologist adjusting the device to optimize sound perception for the individual. Rehabilitation is a crucial phase and involves speech and language therapy to help the brain learn to interpret the new signals from the implant. The length and intensity of rehabilitation vary among individuals, depending on factors such as age, previous experience with sound, and the presence of any additional disabilities.
Benefits and Challenges
The benefits of cochlear implantation are profound for many recipients, offering improved speech recognition, enhanced music appreciation, and increased participation in social and occupational activities. However, the journey to successful cochlear implantation is not without challenges. The adaptation process can be lengthy and requires significant commitment to rehabilitation. Moreover, while cochlear implants can offer a high level of sound perception, they do not restore “normal” hearing and may not eliminate all communication difficulties.
Future Trends and Innovations
The field of cochlear implantation is rapidly evolving, with ongoing research aimed at improving device technology, surgical techniques, and post-operative care. Advances in areas such as electrode design, signal processing algorithms, and the development of totally implantable devices are expected to further enhance the benefits and accessibility of cochlear implants. Additionally, the expansion of candidacy criteria to include individuals with lesser degrees of hearing loss and the exploration of bilateral implantation (implants in both ears) are areas of active investigation, promising to expand the reach and effectiveness of cochlear implant surgery.
Decision Framework for Potential Candidates
For individuals considering cochlear implant surgery, a decision framework that weighs the potential benefits against the challenges and risks is essential. Key factors to consider include the severity of hearing loss, the likelihood of significant improvement with an implant, the commitment required for post-operative rehabilitation, and the potential impact on quality of life. Consulting with healthcare professionals and engaging with support groups or online forums where individuals share their experiences can provide valuable insights into what to expect from the journey.
Case Study: Real-World Applications
A case study of a 35-year-old woman who received a cochlear implant after struggling with severe hearing loss since childhood illustrates the transformative impact of this technology. Pre-implantation, she had difficulty perceiving speech and music, relying heavily on lip-reading and writing for communication. Post-implantation, with intensive speech therapy, she reported significant improvements in speech recognition, both in quiet and noisy environments, and a renewed appreciation for music. Her story underscores the potential of cochlear implantation to not only improve auditory function but to enhance social interaction, emotional well-being, and overall quality of life.
Technical Breakdown: The Technology Behind Cochlear Implants
A closer examination of the technology underlying cochlear implants reveals a complex interplay of engineering, materials science, and neuroscience. The external sound processor, for instance, utilizes advanced signal processing techniques to filter and prioritize sound, mimicking the natural auditory system’s ability to focus on specific sounds amidst background noise. The electrode array, inserted into the cochlea, is designed to stimulate different regions of the auditory nerve, corresponding to various sound frequencies, thereby facilitating the perception of a wide range of sounds. Ongoing technological innovations aim to refine these components, enhancing sound quality and reducing the size and power consumption of the devices.
Myth vs. Reality: Common Misconceptions About Cochlear Implants
Despite the advancements and successes of cochlear implantation, several misconceptions persist. One common myth is that cochlear implants restore hearing to a “normal” state, akin to having perfect hearing without any assistive devices. In reality, while cochlear implants can significantly improve sound perception, they do not eliminate all difficulties with hearing, especially in complex auditory environments. Another misconception is that the surgery is risky and involves a long recovery period. While, like any surgery, there are risks and a recovery period, the majority of individuals undergo the procedure without significant complications and can resume their daily activities within a few weeks.
Conclusion
Cochlear implant surgery represents a groundbreaking intervention for individuals with severe to profound sensorineural hearing loss, offering a path to improved communication, social interaction, and overall quality of life. As technology continues to evolve and our understanding of the auditory system deepens, the potential of cochlear implants to transform lives will only continue to grow. For those considering this life-changing procedure, a thorough understanding of the process, from candidacy evaluation through post-operative rehabilitation, is crucial. With the right support, commitment, and technology, individuals with significant hearing loss can look forward to a future filled with the richness and complexity of sound.
What is the primary criterion for someone to be considered a candidate for cochlear implant surgery?
+The primary criterion is severe to profound sensorineural hearing loss in one or both ears, with limited benefit from traditional hearing aids, and no medical conditions that would pose a risk for the surgery.
How long does it typically take to recover from cochlear implant surgery?
+Most individuals can return home the same day or the day after surgery. The external sound processor is activated about 2-4 weeks after surgery, and full recovery, including rehabilitation, can take several months.
Can cochlear implants restore hearing to a “normal” state?
+No, while cochlear implants can significantly improve sound perception, they do not restore “normal” hearing. Recipients may still experience difficulties, especially in complex auditory environments.
What is involved in the rehabilitation process after cochlear implantation?
+Rehabilitation involves speech and language therapy to help the brain learn to interpret the new signals from the implant. The length and intensity of rehabilitation vary among individuals.
Are there any potential risks or complications associated with cochlear implant surgery?
+Like any surgery, there are risks and potential complications, including infection, facial nerve paralysis, and device failure. However, the majority of procedures are successful without significant complications.