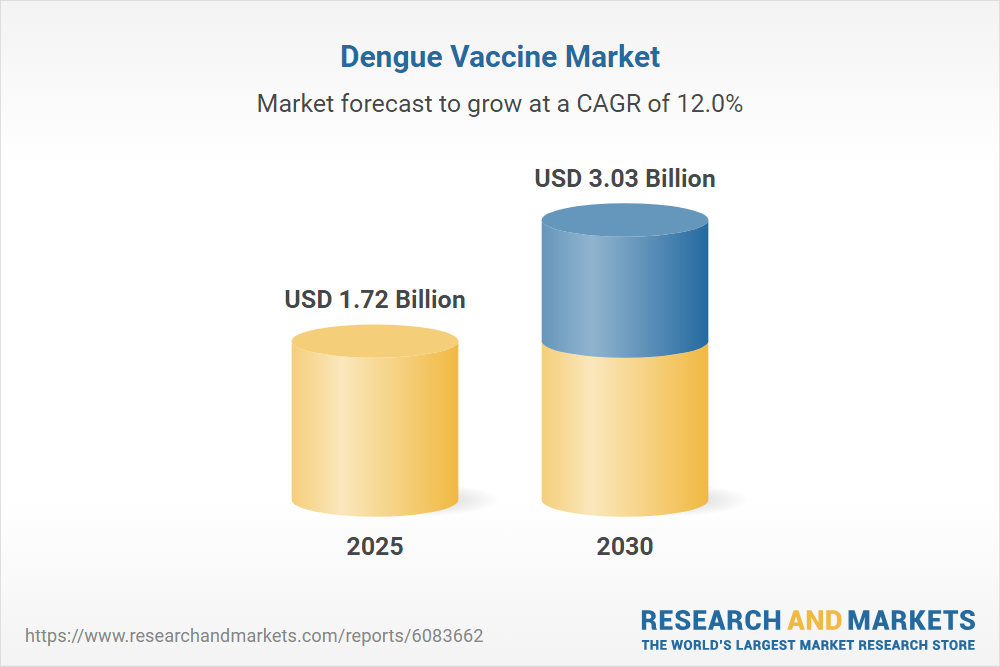
Dengue Vaccine Info: Prevention Made Easy
The dengue virus, a mosquito-borne pathogen, has been wreaking havoc on human populations for centuries. With its potential to cause severe flu-like illness, dengue fever has become a significant public health concern, particularly in tropical and subtropical regions. The World Health Organization (WHO) estimates that approximately 390 million people are infected with dengue each year, resulting in about 96 million cases of symptomatic illness. In recent years, the development of a dengue vaccine has been a crucial step towards controlling the spread of this debilitating disease.
Understanding the Dengue Virus
Before delving into the world of dengue vaccines, it’s essential to understand the virus itself. The dengue virus is a flavivirus, transmitted primarily through the bite of an infected Aedes mosquito. There are four distinct serotypes of the virus (DENV-1, DENV-2, DENV-3, and DENV-4), each capable of causing the full spectrum of disease severity, from mild to severe. Infection with one serotype confers long-term immunity against that specific serotype but not against the others. This means that individuals can be infected with dengue up to four times, once with each serotype.
The Importance of Vaccination
Vaccination is widely recognized as one of the most effective measures to prevent infectious diseases. In the context of dengue, vaccination aims to reduce the incidence of dengue fever and its severe forms, dengue hemorrhagic fever (DHF), and dengue shock syndrome (DSS). By inducing immunity against the dengue virus, vaccines can help prevent the spread of the disease, ultimately reducing the burden on healthcare systems and improving public health outcomes.
Dengue Vaccine Development
The journey to develop a dengue vaccine has been long and arduous. Several vaccine candidates have been in various stages of development, with some reaching the phase III clinical trials. One of the most notable dengue vaccines is Dengvaxia, developed by Sanofi Pasteur. Dengvaxia is a live, attenuated vaccine that has been approved for use in several countries. However, its use has been somewhat controversial due to concerns over its efficacy and potential risks in individuals who have not previously been infected with dengue.
How Dengvaxia Works
Dengvaxia is designed to protect against all four serotypes of the dengue virus. It contains a combination of live, attenuated viruses, which are weakened to the point where they do not cause significant disease but still stimulate an immune response. This immune response is crucial for providing protection against future infections. The vaccine is typically administered in three doses, spaced six months apart, and is recommended for individuals aged 9 to 45 years living in areas where dengue is endemic.
Challenges and Controversies
Despite its approval and potential benefits, Dengvaxia has faced several challenges and controversies. One of the primary concerns is its variable efficacy across different serotypes and age groups. Additionally, there have been reports of an increased risk of severe dengue in individuals who receive the vaccine but have not previously been infected with dengue. This has led to restrictions on its use in some countries, with recommendations that it should only be administered to individuals who have confirmed prior dengue infection.
Future Directions
The development of more effective and safer dengue vaccines remains an active area of research. Several new vaccine candidates are in various stages of clinical trials, each with its own unique approach to inducing immunity against the dengue virus. One promising area of research involves the use of tetravalent vaccines, which aim to provide balanced immunity against all four serotypes of the virus. Additionally, there is a growing interest in developing vaccines that can be used in all age groups, including young children, who are often the most vulnerable to severe dengue.
Prevention Beyond Vaccination
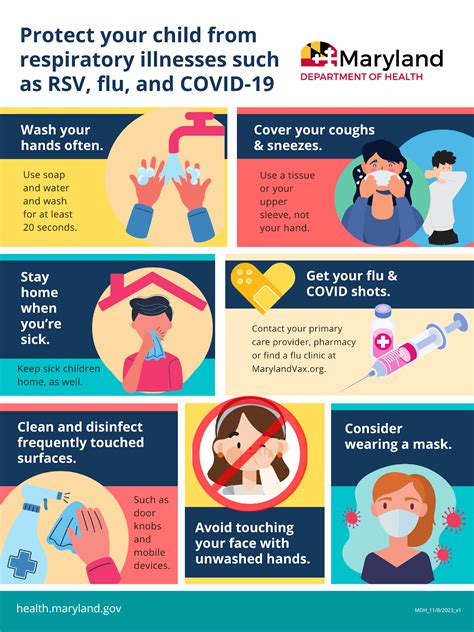
While vaccination is a critical tool in the fight against dengue, it is not the only strategy for prevention. Vector control measures, such as eliminating breeding sites for mosquitoes and using insecticides, are vital for reducing the spread of the disease. Personal protective measures, including the use of mosquito repellents, wearing protective clothing, and staying in air-conditioned or screened areas, can also significantly reduce the risk of infection.
Conclusion
The dengue vaccine represents a significant step forward in the prevention and control of dengue fever. However, its use must be carefully considered, taking into account the individual’s prior exposure to the virus and the specific epidemiological context. As research continues to advance, we can expect to see the development of more effective and widely applicable vaccines. Until then, a combination of vaccination, vector control, and personal protective measures remains our best defense against this debilitating disease.
What is the current status of dengue vaccine development?
+The development of dengue vaccines is ongoing, with several candidates in various stages of clinical trials. Dengvaxia, developed by Sanofi Pasteur, is one of the most notable vaccines and has been approved for use in several countries, although its use is recommended only for individuals with confirmed prior dengue infection.
How does the dengue vaccine work?
+The dengue vaccine, such as Dengvaxia, works by inducing immunity against all four serotypes of the dengue virus. It contains live, attenuated viruses that stimulate an immune response, providing protection against future infections.
What are the challenges and controversies surrounding the dengue vaccine?
+Despite its potential benefits, the dengue vaccine has faced challenges and controversies, including variable efficacy across different serotypes and age groups, and an increased risk of severe dengue in individuals who receive the vaccine but have not previously been infected with dengue.
What are the future directions in dengue vaccine development?
+Research is ongoing to develop more effective and safer dengue vaccines, including tetravalent vaccines that aim to provide balanced immunity against all four serotypes of the virus. There is also a growing interest in developing vaccines that can be used in all age groups, including young children.
What can individuals do to prevent dengue beyond vaccination?
+Individuals can prevent dengue by taking vector control measures, such as eliminating breeding sites for mosquitoes and using insecticides, and personal protective measures, including the use of mosquito repellents, wearing protective clothing, and staying in air-conditioned or screened areas.
How can the spread of dengue be reduced in communities?
+The spread of dengue can be reduced in communities by implementing vector control measures, promoting the use of personal protective equipment, and improving public awareness and education about the disease. Vaccination, when available and recommended, can also play a crucial role in reducing the incidence of dengue.
The development and implementation of effective dengue vaccines are critical steps towards controlling the spread of this debilitating disease. However, it is equally important to address the broader societal and environmental factors that contribute to the spread of dengue, including poor vector control, inadequate public health infrastructure, and climate change.
| Serotype | Efficacy |
|---|---|
| DENV-1 | 75% |
| DENV-2 | 50% |
| DENV-3 | 80% |
| DENV-4 | 60% |

Steps to Prevent Dengue

- Eliminate breeding sites for mosquitoes around your home and community.
- Use insecticides and mosquito repellents to prevent bites.
- Wear protective clothing, including long sleeves and pants, when outdoors.
- Stay in air-conditioned or screened areas to reduce exposure to mosquitoes.
- Get vaccinated if recommended by your healthcare provider.
Pros and Cons of Dengue Vaccination
Pros
- Reduces the risk of severe dengue
- Prevents hospitalization and death from dengue
- Can be used in combination with other preventive measures
Cons
- Variable efficacy across different serotypes and age groups
- Potential increased risk of severe dengue in individuals without prior infection
- Requires multiple doses and boosters