Diabetes Blood Sugar Levels
Maintaining optimal blood sugar levels is crucial for individuals with diabetes to prevent complications and ensure overall health. Blood sugar levels, also known as blood glucose levels, refer to the amount of glucose present in the blood at a given time. Glucose is a type of sugar that serves as the primary source of energy for the body’s cells. In individuals with diabetes, the body either cannot produce enough insulin, a hormone that regulates blood sugar levels, or cannot effectively use the insulin it produces. As a result, blood sugar levels can become elevated, leading to a range of health problems.
Understanding Blood Sugar Levels
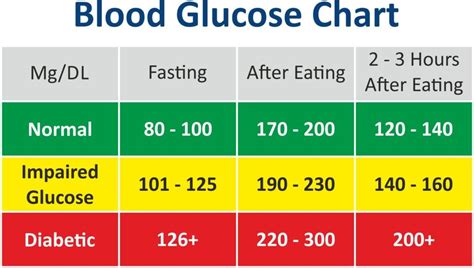
To manage diabetes effectively, it’s essential to understand the different blood sugar level ranges and their implications. The American Diabetes Association (ADA) recommends the following blood sugar level targets for individuals with diabetes:
- Fasting blood sugar levels: 80-130 mg/dL
- Before meals: Less than 130 mg/dL
- After meals: Less than 180 mg/dL
- At bedtime: 100-140 mg/dL
These targets may vary depending on factors such as age, other health conditions, and the type of diabetes. For instance, pregnant women with diabetes may have more stringent targets to protect the health of both mother and baby.
Factors Influencing Blood Sugar Levels
Several factors can influence blood sugar levels, including:
Diet: Consuming high-carbohydrate foods can cause blood sugar levels to rise. Foods with a high glycemic index (GI) are particularly effective at raising blood sugar levels because they are quickly broken down into glucose during digestion.
Physical Activity: Regular physical activity can help lower blood sugar levels by increasing the body’s sensitivity to insulin. However, intense or prolonged exercise can sometimes cause blood sugar levels to rise due to the release of stress hormones like adrenaline.
Medications: Certain medications, including diabetes medications, can affect blood sugar levels. It’s crucial to follow the prescribed regimen and monitor blood sugar levels regularly to adjust the dosage as needed.
Stress and Sleep: Chronic stress and inadequate sleep can raise blood sugar levels by increasing the production of stress hormones, which can lead to insulin resistance.
Hormonal Changes: Hormonal fluctuations during menstruation, pregnancy, or menopause can affect blood sugar levels. Women with diabetes should work closely with their healthcare provider to adjust their diabetes management plan as needed during these times.
Monitoring Blood Sugar Levels
Regular monitoring of blood sugar levels is a critical component of diabetes management. This can be done using a blood glucose meter, which involves pricking the finger with a lancet to collect a small blood sample. The sample is then placed on a test strip, and the meter provides a reading of the current blood glucose level.
For individuals with type 1 diabetes and some with type 2 diabetes, a continuous glucose monitor (CGM) may be recommended. A CGM is a small device that is inserted under the skin to continuously track glucose levels throughout the day and night, providing valuable insights into how different activities and foods affect blood sugar levels.
Managing Blood Sugar Levels
Effective management of blood sugar levels involves a combination of lifestyle modifications and, when necessary, medication. Key strategies include:
- Healthy Eating: Following a balanced diet that is low in added sugars, saturated fats, and sodium, and high in fruits, vegetables, whole grains, and lean proteins.
- Regular Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, along with muscle-strengthening activities at least twice a week.
- Stress Management: Practicing stress-reducing techniques such as meditation, yoga, or deep breathing exercises.
- Adequate Sleep: Aiming for 7-8 hours of sleep per night to help regulate blood sugar levels and insulin sensitivity.
- Medication Adherence: Taking diabetes medications as prescribed by a healthcare provider.
Complications of Unmanaged Blood Sugar Levels
Failure to manage blood sugar levels can lead to a range of serious health complications, including:
- Diabetic Ketoacidosis (DKA): A life-threatening condition that occurs when the body produces high levels of blood acids called ketones.
- Hyperosmolar Hyperglycemic State (HHS): A serious condition that occurs when the blood sugar levels are very high, causing the body to lose a lot of water.
- Nerve Damage (Neuropathy): High blood sugar levels can damage the nerves, leading to numbness, tingling, and pain in the hands and feet.
- Kidney Damage (Nephropathy): Diabetes is the leading cause of kidney failure, which can require dialysis or a kidney transplant.
- Blindness (Retinopathy): High blood sugar levels can damage the blood vessels in the retina, leading to vision loss and potentially blindness.
- Foot Damage: Nerve damage and poor circulation can lead to serious foot problems, such as ulcers and infections, which can sometimes require amputation.
Conclusion
Maintaining optimal blood sugar levels is a critical aspect of diabetes management, requiring a multifaceted approach that includes a healthy diet, regular physical activity, stress management, adequate sleep, and adherence to medication regimens. By understanding the factors that influence blood sugar levels and implementing effective management strategies, individuals with diabetes can reduce their risk of developing serious health complications and improve their overall quality of life.
What are the normal blood sugar levels for individuals with diabetes?
+Normal blood sugar levels for individuals with diabetes can vary, but general targets include fasting levels between 80-130 mg/dL, before meals less than 130 mg/dL, after meals less than 180 mg/dL, and at bedtime between 100-140 mg/dL. However, these targets may be adjusted based on individual factors.
How often should blood sugar levels be checked?
+The frequency of checking blood sugar levels depends on the type of diabetes, the presence of other health conditions, and the effectiveness of the current diabetes management plan. Individuals with type 1 diabetes or those using insulin typically need to check their blood sugar levels more frequently than those with type 2 diabetes who are not on insulin.
Can diet and exercise alone control blood sugar levels for everyone with diabetes?
+For some individuals with type 2 diabetes, particularly those who are newly diagnosed or have mild diabetes, diet and exercise may be sufficient to control blood sugar levels. However, many people with diabetes, especially those with type 1 diabetes or advanced type 2 diabetes, will require medication or insulin therapy in addition to lifestyle modifications to manage their blood sugar levels effectively.
What are the most common complications of unmanaged diabetes?
+The most common complications of unmanaged diabetes include heart disease, stroke, kidney damage, nerve damage, and vision problems, including blindness. Effective management of blood sugar levels can significantly reduce the risk of developing these complications.
How can individuals with diabetes manage stress to help control their blood sugar levels?
+Stress management techniques such as meditation, yoga, deep breathing exercises, and spending time in nature can help individuals with diabetes control their stress levels, which in turn can help regulate blood sugar levels. Regular physical activity and getting enough sleep are also crucial for managing stress and blood sugar levels.
By adopting a comprehensive approach to managing blood sugar levels and staying informed about the latest developments in diabetes care, individuals with diabetes can lead active, healthy lives and reduce their risk of complications. Regular monitoring, a balanced lifestyle, and adherence to medication regimens are key components of effective diabetes management.



