Diabetes Eye Care: Comprehensive Exam Checklist
Diabetes is a chronic condition that affects millions of people worldwide, and one of its most significant complications is its impact on eye health. High blood sugar levels can damage the blood vessels in the retina, leading to a condition known as diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness, making regular eye exams crucial for people with diabetes. A comprehensive eye exam for diabetes includes several key components, which are outlined in this checklist.
Introduction to Diabetic Retinopathy
Diabetic retinopathy is a condition characterized by the damage it causes to the blood vessels in the retina, which is the light-sensitive tissue at the back of the eye. This damage can lead to leaks, causing the retinal tissue to swell, or it can lead to the growth of new, fragile blood vessels that can bleed easily, causing vision problems. The severity of diabetic retinopathy can vary, ranging from mild non-proliferative diabetic retinopathy (NPDR) to more severe proliferative diabetic retinopathy (PDR).
Comprehensive Exam Components
A comprehensive diabetic eye exam is designed to detect any signs of diabetic retinopathy or other diabetes-related eye problems early, when they are more treatable. The components of this exam include:
Visual Acuity Test: This is a standard test that measures the sharpness of your vision. During the test, you’ll be asked to read from an eye chart to determine how well you can see objects at a distance.
Dilated Eye Exam: This involves the use of eye drops to widen your pupils, allowing the doctor to see the back of your eyes more clearly. The doctor will then use a special lens to examine the retina and optic nerve for signs of damage.
Retinoscopy: This test is used to determine the correct lens prescription. It involves shining a light into the eye and observing how it reflects off the retina.
Slit Lamp Exam: A slit lamp is a microscope with a light source that allows the doctor to examine the structures at the front of the eye, including the eyelids, lashes, iris, and lens.
Optical Coherence Tomography (OCT): This non-invasive imaging test uses low-coherence interferometry to capture micrometer-resolution, three-dimensional images from within optical scattering media (e.g., biological tissue). In the context of diabetic retinopathy, OCT is used to visualize the retina, helping to identify areas of thickening or fluid accumulation.
Fluorescein Angiography: For this test, a special dye is injected into a vein in your arm. The dye circulates through your body and into your eyes, where it highlights the blood vessels in the retina, making them easier to see. A special camera takes pictures of your retina as the dye circulates, allowing the doctor to see any leaking or abnormal blood vessels.
Importance of Regular Exams
The key to managing diabetic retinopathy and preventing vision loss is early detection and treatment. The American Diabetes Association recommends that people with type 1 diabetes have an initial comprehensive eye exam by an ophthalmologist or optometrist within five years of their diabetes diagnosis, and people with type 2 diabetes should have an eye exam shortly after their diabetes diagnosis. If the exam is normal, the ADA recommends exams every 1-3 years, depending on the risk factors for progression. More frequent exams are recommended for pregnant women with diabetes due to the increased risk of diabetic retinopathy during pregnancy.
Treatment Options
Treatment for diabetic retinopathy depends on its severity. For mild cases, no treatment may be necessary, but regular monitoring is crucial. For more advanced cases, treatment options include:
Laser Surgery: To reduce swelling, to stop or slow the growth of new, fragile blood vessels, or to destroy areas of the retina where new blood vessels have grown.
Vitrectomy: A surgery to remove blood and scar tissue from the vitreous gel at the center of the eye, which can help to restore vision.
Medications: Injected into the eye to reduce swelling or to stop the growth of new, fragile blood vessels.
Prevention and Management
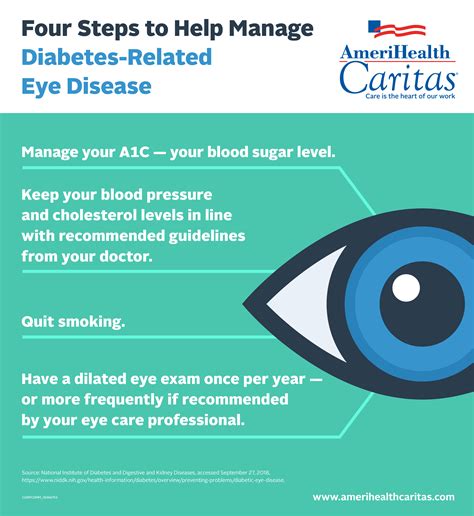
While some risk factors for diabetic retinopathy, such as the duration of diabetes and genetics, cannot be changed, there are steps that can be taken to reduce the risk of developing diabetic retinopathy or to slow its progression. These include:
Maintaining Good Blood Sugar Control: High blood sugar levels can damage blood vessels in the retina, so keeping blood sugar levels within a target range can help to reduce this risk.
Monitoring Blood Pressure and Cholesterol: High blood pressure and high cholesterol can also impact the health of blood vessels in the retina, so managing these conditions is important.
Avoiding Smoking: Smoking can increase the risk of many health problems, including diabetic retinopathy.
Regular Eye Exams: Early detection and treatment are key to preventing vision loss from diabetic retinopathy, so attending regular eye exams as recommended by your healthcare provider is essential.
Conclusion
Diabetes can have a significant impact on eye health, but with the right care and attention, many of the related eye problems can be prevented or managed effectively. A comprehensive diabetic eye exam is a crucial tool in this management, allowing for the early detection and treatment of diabetic retinopathy and other diabetes-related eye conditions. By understanding the components of a comprehensive eye exam and the importance of regular exams, individuals with diabetes can take proactive steps to protect their vision and maintain their overall eye health.
Step-by-Step Guide to Preparing for a Comprehensive Diabetic Eye Exam
- Schedule the Exam: Make sure to schedule your comprehensive diabetic eye exam with an ophthalmologist or optometrist as recommended by your healthcare provider.
- Bring Necessary Information: Write down your medical history, including when you were diagnosed with diabetes, any previous treatments for diabetic retinopathy, and any medications you're currently taking.
- Prepare Questions: Come prepared with questions or concerns you have about your eye health or the exam process.
- Arrive Early: Plan to arrive a little early to fill out any necessary paperwork and to get settled before your exam.
- Understand the Results: After the exam, ask your doctor to explain the results, including any findings related to diabetic retinopathy, and discuss any necessary follow-up appointments or treatments.
Frequently Asked Questions
How often should I get a comprehensive eye exam if I have diabetes?
+The frequency of comprehensive eye exams if you have diabetes can vary based on your specific health needs and risk factors. Generally, the American Diabetes Association recommends that people with type 1 diabetes have an initial comprehensive eye exam by an ophthalmologist or optometrist within five years of their diabetes diagnosis. For those with type 2 diabetes, an eye exam is recommended shortly after diagnosis. If the initial exam is normal, follow-up exams are usually recommended every 1-3 years.
Can diabetic retinopathy be treated if it's detected early?
+Yes, early detection of diabetic retinopathy can significantly improve treatment outcomes. While there's no cure for diabetic retinopathy, treatments such as laser surgery, medications, and vitrectomy can help to reduce vision loss and, in some cases, restore vision. Regular eye exams are crucial for detecting diabetic retinopathy in its early stages when it is most treatable.
How does diabetes affect eye health beyond diabetic retinopathy?
+Diabetes can affect eye health in several ways beyond diabetic retinopathy. For instance, high blood sugar levels can cause the lens in the eye to swell, leading to blurred vision, which usually improves once blood sugar levels are under control. Diabetes also increases the risk of cataracts and glaucoma. Regular eye exams can help to detect these conditions early, improving the effectiveness of treatment.
Are there any new advancements in the treatment of diabetic retinopathy?
+Yes, there are ongoing advancements in the treatment of diabetic retinopathy. For example, intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) drugs have become a common treatment for diabetic macular edema, a complication of diabetic retinopathy. Additionally, research into new pharmacological therapies and surgical techniques continues, aiming to improve treatment efficacy and reduce the risk of complications.
By understanding the importance of comprehensive diabetic eye exams and following the recommended guidelines for examination frequency, individuals with diabetes can play a proactive role in protecting their vision and maintaining their eye health. Regular exams combined with good diabetes management can significantly reduce the risk of vision loss due to diabetic retinopathy.