Diabetes Glucose Levels
Understanding diabetes and glucose levels is crucial for managing the condition effectively. Diabetes is a chronic health condition that affects how your body turns food into energy. It’s primarily characterized by high blood sugar levels, which can lead to a variety of serious health problems if not managed properly. The key to controlling diabetes is understanding how different factors affect blood glucose levels and learning how to keep these levels within a target range.
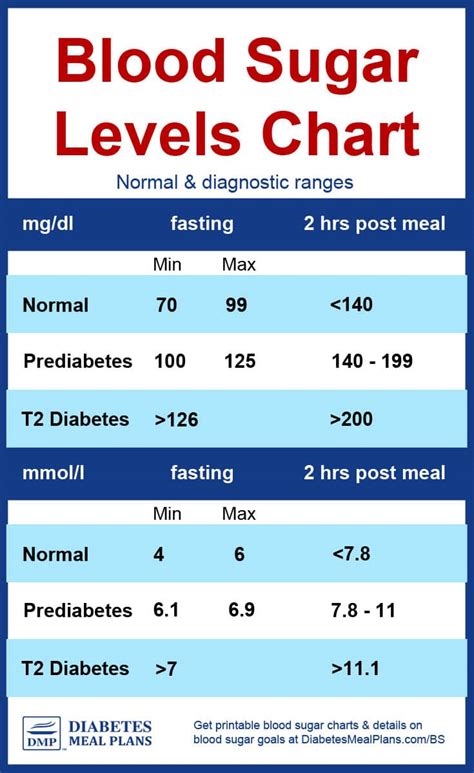
What are Normal Glucose Levels?
Normal blood glucose levels vary throughout the day, but ideally, they should be between 70 and 140 mg/dL (milligrams per deciliter) for people without diabetes. For individuals with diabetes, the target glucose levels are slightly different and can vary depending on the time of day and other factors such as medication, diet, and physical activity. Generally, the American Diabetes Association recommends the following targets for blood glucose levels: - Before meals: 80 to 130 mg/dL - After meals (1-2 hours after beginning of meal): Less than 180 mg/dL
Factors Affecting Glucose Levels
Several factors can affect blood glucose levels, including: 1. Diet and Nutrition: The types and amounts of food you eat, especially carbohydrates, can significantly impact your blood glucose levels. Foods that are high in fiber and have a low glycemic index can help stabilize glucose levels. 2. Physical Activity: Regular exercise can lower your blood glucose levels and improve your body’s insulin sensitivity. This means your body needs less insulin to manage your blood glucose. 3. Medications: People with diabetes often use medications, including insulin and oral medications, to manage their blood glucose levels. The type and dosage of medication can affect glucose levels. 4. Stress: Stress can raise your blood glucose levels by releasing hormones like cortisol and adrenaline, which prepare your body to fight or flee, thereby increasing glucose release from energy stores. 5. Sleep and Illness: Lack of quality sleep and being ill can also impact blood glucose levels. Poor sleep can increase levels of stress hormones, raising blood glucose, and illness can make your body produce more glucose.
Importance of Monitoring Glucose Levels
Monitoring your glucose levels regularly helps you understand how different factors affect your levels and enables you to make informed decisions about diet, exercise, and medication. It’s a critical component of diabetes management. For instance, checking your glucose levels before meals can help you decide how much insulin to take or how to adjust your diet and physical activity for better glucose control.
Tools for Monitoring Glucose Levels
There are several tools available for monitoring glucose levels: 1. Blood Glucose Meters: These are small devices that you use with test strips to measure your blood glucose level. They are the most common method of glucose monitoring. 2. Continuous Glucose Monitors (CGMs): These devices measure glucose levels throughout the day and night. They involve a small sensor inserted under the skin, usually on the abdomen or back of the arm, and can provide real-time glucose readings. 3. Flash Glucose Monitoring Systems: Similar to CGMs, these devices also involve a sensor under the skin but do not require calibration with fingerstick tests. They provide glucose readings when you scan the sensor with a reader or compatible smartphone.
Managing High and Low Blood Sugar
Managing high and low blood sugar levels is crucial for preventing complications and maintaining quality of life. High blood sugar, or hyperglycemia, can occur due to skipped insulin doses, eating more carbohydrates than planned, or being less active than usual. Symptoms include increased thirst and urination, blurred vision, and headaches. Low blood sugar, or hypoglycemia, can occur due to too much insulin, skipped meals, or unusual physical activity. Symptoms include shakiness, dizziness, sweating, hunger, irritability, confusion, or feeling jittery.
Practical Management Tips
- Keep a Record: Maintain a log or use an app to track your glucose levels, physical activity, meals, and medications. This helps identify patterns and understand what affects your levels.
- Be Active: Regular physical activity can help lower blood glucose levels and improve overall health.
- Eat Wisely: Focus on nutrient-dense foods like vegetables, fruits, whole grains, lean proteins, and healthy fats. Limit foods that are high in sugar, salt, and unhealthy fats.
- Stay Hydrated: Drinking enough water can help your body regulate blood sugar levels and prevent dehydration, a common complication of high blood sugar.
Long-Term Complications of Unmanaged Diabetes
If left unmanaged, diabetes can lead to serious long-term complications, including heart disease, stroke, kidney disease, nerve damage, vision problems including blindness, and foot damage possibly leading to amputation. Pregnant women with unmanaged diabetes also have a higher risk of pregnancy complications.
Emotional and Mental Health Considerations
Living with diabetes can also affect your emotional and mental health. The constant need to monitor and manage your condition, along with potential fears about complications, can lead to feelings of frustration, anxiety, and depression. It’s essential to address these feelings and seek support from healthcare providers, family, friends, or support groups.
Future Trends in Diabetes Management
Advancements in technology and medical science are continually improving diabetes management. Emerging trends include more sophisticated continuous glucose monitoring systems, insulin pumps with automated insulin adjustment, and mobile apps that integrate glucose data with insulin dosing advice and lifestyle management. Research into new medications and potential cures, such as islet cell transplantation and stem cell therapies, also offers hope for the future.
Resource Guide
For individuals looking to learn more about managing their diabetes and controlling glucose levels, there are numerous resources available: - American Diabetes Association (ADA): Provides comprehensive information on diabetes management, including diet, exercise, and medication. - Centers for Disease Control and Prevention (CDC): Offers resources on diabetes prevention and management. - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Conducts and supports research on diabetes and provides information on managing the condition. - Local Support Groups: Many communities have support groups for people with diabetes, offering a platform to share experiences and learn from others.
Decision Framework for Diabetes Management
When making decisions about diabetes management, consider the following framework: 1. Set Clear Goals: Define what you want to achieve in terms of glucose control, weight management, and overall health. 2. Assess Your Current Situation: Evaluate your diet, physical activity level, medication adherence, and glucose monitoring habits. 3. Explore Options: Look into different diet plans, exercise programs, and medication options that could help you meet your goals. 4. Consult Professionals: Discuss your plans with your healthcare provider to ensure they are safe and appropriate for your specific situation. 5. Implement Changes Gradually: Making gradual changes can be more sustainable than trying to overhaul everything at once. 6. Monitor Progress: Regularly check your glucose levels and adjust your plan as necessary to stay on track.
FAQ Section
What are the common symptoms of diabetes?
+Common symptoms include increased thirst and urination, feeling tired, blurred vision, slow healing of cuts and wounds, and tingling or numbness in the hands and feet. However, some people with diabetes may not exhibit any noticeable symptoms, especially in the early stages.
How often should I check my blood glucose levels?
+The frequency of checking blood glucose levels depends on the type of diabetes you have and your treatment plan. Generally, people with diabetes are advised to check their levels at least four times a day, but this can vary. It's best to follow the advice of your healthcare provider.
Can diabetes be cured?
+Currently, there is no cure for diabetes, but it can be managed effectively with medication, diet, and exercise. Researchers are working on potential cures, such as islet cell transplantation and stem cell therapies, but these are still in the experimental stages.
How can I prevent complications from diabetes?
+Managing your blood glucose levels, having regular check-ups with your healthcare provider, maintaining a healthy diet, exercising regularly, and not smoking can help prevent complications. It's also crucial to monitor your blood pressure and cholesterol levels.
Can I still eat sweets if I have diabetes?
+Yes, but in moderation. People with diabetes can still enjoy sweets as part of a balanced diet. It's essential to consider the carbohydrate and sugar content and factor it into your meal planning and insulin dosage if necessary.
In conclusion, managing diabetes effectively requires a comprehensive approach that includes understanding your condition, monitoring glucose levels, making informed dietary and lifestyle choices, and staying up-to-date with the latest advancements in diabetes care. By taking proactive steps and working closely with healthcare professionals, individuals with diabetes can lead active, healthy lives and reduce the risk of long-term complications.