Diabetes Management: Expert Guide To Normal Range
Maintaining a normal blood sugar range is crucial for individuals with diabetes to prevent complications and ensure overall health. Diabetes management involves a multifaceted approach, including lifestyle modifications, medication, and continuous monitoring. Understanding what constitutes a normal range and how to achieve it is essential for effective diabetes care.
Understanding Blood Sugar Levels
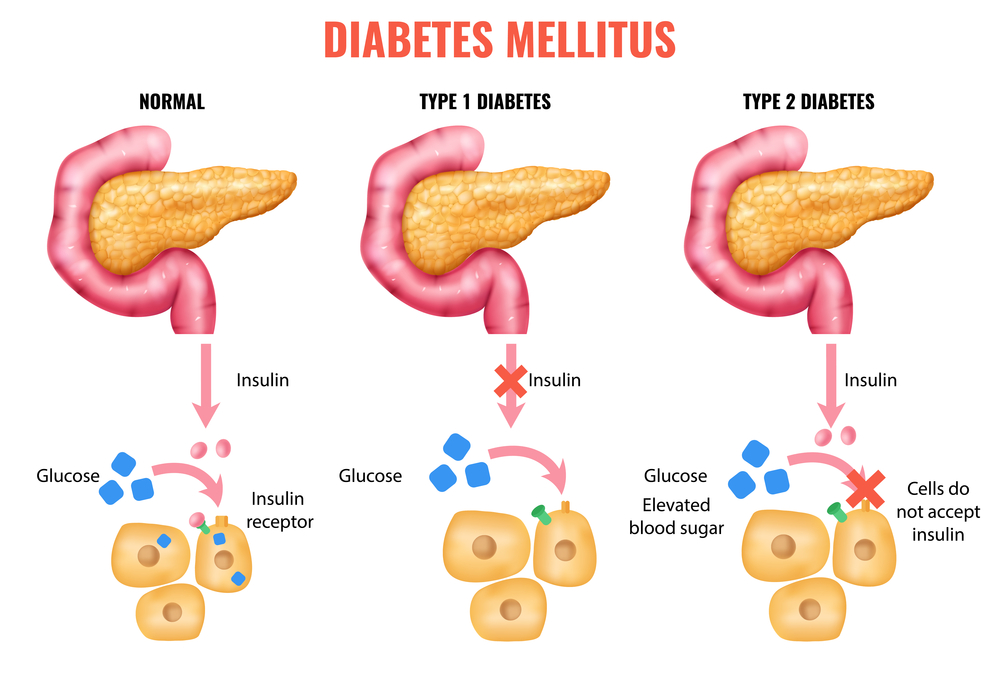
Blood sugar levels, measured in milligrams per deciliter (mg/dL), indicate the amount of glucose present in the blood. The body regulates blood sugar levels through the release of insulin and glucagon, hormones produced by the pancreas. In individuals with diabetes, this regulatory mechanism is impaired, leading to elevated blood sugar levels.
Normal Blood Sugar Range
The normal blood sugar range varies throughout the day, depending on factors such as meal times and physical activity. The American Diabetes Association (ADA) provides the following guidelines for normal blood sugar levels:
- Fasting blood sugar: Less than 100 mg/dL
- Before meals: 70-130 mg/dL
- After meals: Less than 180 mg/dL
- At bedtime: 100-140 mg/dL
Achieving and maintaining these target ranges can significantly reduce the risk of diabetes-related complications, such as heart disease, kidney damage, and nerve damage.
Lifestyle Modifications for Diabetes Management
Lifestyle modifications play a critical role in managing diabetes and achieving a normal blood sugar range. Key strategies include:
- Dietary Changes: Following a balanced diet that is low in sugar, salt, and unhealthy fats can help regulate blood sugar levels. Foods rich in fiber, such as fruits, vegetables, and whole grains, are particularly beneficial.
- Physical Activity: Regular exercise, such as walking, cycling, or swimming, can improve insulin sensitivity, reducing blood sugar levels. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
- Weight Management: Maintaining a healthy weight through a combination of diet and exercise can significantly improve insulin sensitivity and glucose metabolism.
- Stress Management: Chronic stress can raise blood sugar levels. Engaging in stress-reducing activities, such as yoga, meditation, or deep breathing exercises, can help mitigate this effect.
Medication and Monitoring
In addition to lifestyle modifications, medication and continuous monitoring are crucial components of diabetes management.
- Medication Adherence: Taking prescribed medications as directed is essential for maintaining blood sugar control. This may include metformin, sulfonylureas, or insulin therapy, depending on the type and severity of diabetes.
- Blood Glucose Monitoring: Regularly monitoring blood sugar levels helps track progress, identify patterns, and make informed decisions about diet, exercise, and medication.
- Continuous Glucose Monitoring (CGM) Systems: CGM systems provide real-time glucose data, enabling more precise management of blood sugar levels and reducing the risk of hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar).
Advanced Technologies in Diabetes Management
Recent advancements in technology have revolutionized diabetes care, offering more precise and convenient management options.
- Insulin Pumps: These devices deliver continuous insulin basal rates and bolus doses, mimicking natural insulin release.
- Smart Insulin Pens: Equipped with memory and calculation functions, smart pens simplify insulin dosing and tracking.
- Artificial Pancreas Systems: These automated systems integrate CGM data with insulin pump therapy, adjusting insulin delivery in real-time to maintain target blood sugar ranges.
Overcoming Challenges in Diabetes Management
Diabetes management can be challenging, with common obstacles including:
- Adherence to Treatment Plans: Sticking to medication regimens, dietary recommendations, and exercise plans can be difficult, particularly in the face of busy schedules or lack of support.
- Emotional and Psychological Factors: Diabetes can have a significant emotional impact, leading to stress, anxiety, or depression. Seeking professional help and connecting with support groups can provide valuable resources and coping strategies.
- Access to Healthcare and Resources: Barriers to healthcare access, including cost, location, and insurance coverage, can hinder effective diabetes management. Exploring local resources, such as community clinics or online support services, can help bridge these gaps.
Future Directions in Diabetes Care
Emerging trends and technologies promise to further enhance diabetes management, including:
- Personalized Medicine: Tailoring treatment plans to individual genetic profiles, lifestyle, and preferences may improve outcomes and adherence.
- Telehealth Services: Virtual consultations and remote monitoring can increase access to diabetes care, particularly for underserved populations.
- Immunotherapy and Regenerative Medicine: Ongoing research into immune system modulation and pancreatic islet cell regeneration may offer new avenues for diabetes prevention and cure.
Conclusion
Achieving a normal blood sugar range is a critical aspect of diabetes management, requiring a comprehensive approach that incorporates lifestyle modifications, medication, and continuous monitoring. By understanding the factors that influence blood sugar levels and leveraging advanced technologies and treatment options, individuals with diabetes can effectively manage their condition, reducing the risk of complications and improving overall quality of life.
What are the normal blood sugar levels for individuals with diabetes?
+For individuals with diabetes, normal blood sugar levels are typically considered to be between 70-130 mg/dL before meals and less than 180 mg/dL after meals. Fasting blood sugar levels should be less than 100 mg/dL, and bedtime levels should range from 100-140 mg/dL.
How often should I monitor my blood sugar levels if I have diabetes?
+The frequency of blood sugar monitoring depends on the type of diabetes, treatment plan, and individual circumstances. Generally, individuals with type 1 diabetes or those using insulin therapy should check their blood sugar levels at least 4-6 times a day. Those with type 2 diabetes not on insulin may need to check less frequently, typically 1-3 times a day, or as recommended by their healthcare provider.
Can lifestyle changes alone manage diabetes without medication?
+For some individuals, particularly those with prediabetes or newly diagnosed type 2 diabetes, lifestyle changes such as diet, exercise, and weight loss may be sufficient to manage blood sugar levels without medication. However, this depends on the severity of diabetes, individual health status, and the effectiveness of these lifestyle modifications in achieving and maintaining target blood sugar ranges. Consultation with a healthcare provider is necessary to determine the best approach.