Diabetic Autonomic Neuropathy
Diabetic autonomic neuropathy (DAN) is a serious and often overlooked complication of diabetes that affects the autonomic nervous system. The autonomic nervous system is responsible for controlling involuntary functions of the body, such as heart rate, blood pressure, digestion, and bowel movements. In people with diabetes, high blood sugar levels over a long period can damage the nerves that make up the autonomic nervous system, leading to a range of symptoms and potentially life-threatening complications.
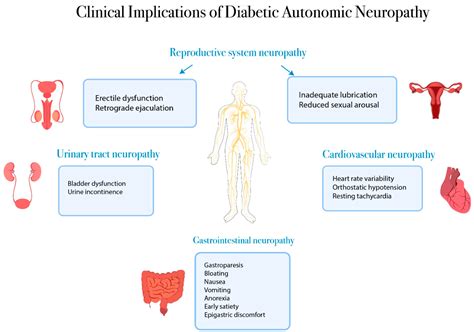
One of the primary concerns with DAN is its impact on the cardiovascular system. Damaged nerves can disrupt the normal functioning of the heart, leading to abnormalities in heart rate and blood pressure. This can result in a range of symptoms, including dizziness, lightheadedness, and fainting spells. In severe cases, DAN can increase the risk of sudden cardiac death, as the damaged nerves can disrupt the heart’s ability to respond to stress and other stimuli.
In addition to its impact on the cardiovascular system, DAN can also affect the digestive system. Damaged nerves can slow down or speed up the movement of food through the digestive tract, leading to symptoms such as nausea, vomiting, diarrhea, and constipation. Some people with DAN may also experience abdominal pain, bloating, and difficulty swallowing.
Another significant concern with DAN is its impact on the genitourinary system. Damaged nerves can disrupt the normal functioning of the bladder, leading to symptoms such as urinary incontinence, frequent urination, and difficulty starting or stopping the flow of urine. In men, DAN can also cause erectile dysfunction, while in women, it can lead to vaginal dryness and decreased libido.
Furthermore, DAN can also affect the respiratory system, leading to symptoms such as shortness of breath, wheezing, and coughing. In severe cases, it can increase the risk of respiratory failure, as the damaged nerves can disrupt the normal functioning of the diaphragm and other respiratory muscles.
The diagnosis of DAN can be challenging, as its symptoms can be similar to those of other conditions. However, a thorough medical history, physical examination, and diagnostic tests such as electrocardiogram (ECG), electromyography (EMG), and nerve conduction studies (NCS) can help confirm the diagnosis. In some cases, a tilt table test may also be used to assess the body’s response to changes in position and to evaluate the autonomic nervous system’s function.
Once diagnosed, the treatment of DAN typically focuses on managing its symptoms and preventing further nerve damage. This can include medications to control blood sugar levels, as well as medications to manage specific symptoms such as orthostatic hypotension, gastrointestinal disturbances, and genitourinary problems. In some cases, pacemakers or other implantable devices may be used to regulate heart rate and blood pressure.
Lifestyle modifications can also play a crucial role in managing DAN. This can include maintaining good blood sugar control, engaging in regular exercise, and practicing stress-reducing techniques such as meditation and deep breathing. Additionally, avoiding activities that can exacerbate symptoms, such as standing for long periods or eating large meals, can also help alleviate symptoms.
In terms of prevention, maintaining good blood sugar control is critical in preventing or delaying the onset of DAN. This can be achieved through a combination of medications, lifestyle modifications, and regular monitoring of blood sugar levels. Additionally, regular check-ups with a healthcare provider can help identify any potential problems early on, allowing for prompt treatment and management.
It’s also important to note that DAN can have a significant impact on a person’s quality of life. The symptoms and complications associated with DAN can lead to decreased mobility, increased risk of falls, and decreased ability to perform daily activities. Furthermore, the emotional and psychological burden of living with a chronic condition can also take a significant toll on mental health and well-being.
Early recognition and treatment of DAN are critical in preventing long-term damage and improving outcomes. Healthcare providers should be aware of the potential for DAN in people with diabetes and take a proactive approach to screening and management.
In conclusion, diabetic autonomic neuropathy is a serious and often overlooked complication of diabetes that can have a significant impact on a person’s quality of life. Its symptoms and complications can be challenging to manage, but with prompt diagnosis, treatment, and lifestyle modifications, it is possible to alleviate symptoms and prevent further nerve damage. By maintaining good blood sugar control, engaging in regular exercise, and practicing stress-reducing techniques, individuals with diabetes can reduce their risk of developing DAN and improve their overall health and well-being.
What are the symptoms of diabetic autonomic neuropathy?
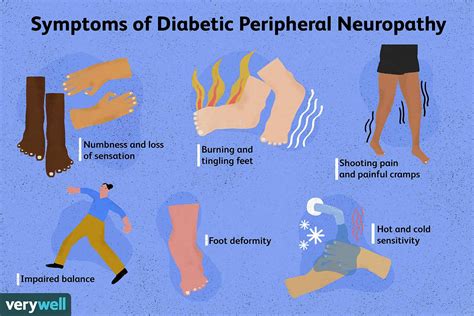
+The symptoms of diabetic autonomic neuropathy can vary depending on the nerves affected, but common symptoms include dizziness, lightheadedness, fainting spells, nausea, vomiting, diarrhea, constipation, abdominal pain, bloating, difficulty swallowing, urinary incontinence, frequent urination, and difficulty starting or stopping the flow of urine.
How is diabetic autonomic neuropathy diagnosed?
+Diabetic autonomic neuropathy can be diagnosed through a thorough medical history, physical examination, and diagnostic tests such as electrocardiogram (ECG), electromyography (EMG), and nerve conduction studies (NCS). In some cases, a tilt table test may also be used to assess the body's response to changes in position and to evaluate the autonomic nervous system's function.
What is the treatment for diabetic autonomic neuropathy?
+The treatment for diabetic autonomic neuropathy typically focuses on managing its symptoms and preventing further nerve damage. This can include medications to control blood sugar levels, as well as medications to manage specific symptoms such as orthostatic hypotension, gastrointestinal disturbances, and genitourinary problems.
Steps to Manage Diabetic Autonomic Neuropathy
- Maintain good blood sugar control through a combination of medications, lifestyle modifications, and regular monitoring of blood sugar levels.
- Engage in regular exercise to improve cardiovascular health and reduce the risk of falls.
- Practice stress-reducing techniques such as meditation and deep breathing to manage stress and anxiety.
- Avoid activities that can exacerbate symptoms, such as standing for long periods or eating large meals.
- Stay hydrated by drinking plenty of water and avoiding sugary drinks.
Benefits and Drawbacks of Medications for Diabetic Autonomic Neuropathy
| Medication | Benefits | Drawbacks |
|---|---|---|
| Fludrocortisone | Helps to regulate blood pressure and improve orthostatic tolerance | Can cause fluid retention, hypertension, and hypokalemia |
| Midodrine | Helps to improve blood pressure and reduce symptoms of orthostatic hypotension | Can cause headaches, dizziness, and gastrointestinal disturbances |
| Pyridostigmine | Helps to improve gastrointestinal motility and reduce symptoms of gastroparesis | Can cause nausea, vomiting, and diarrhea |