Diabetic Autonomic Neuropathy: Manage Your Symptoms
Living with diabetes can be challenging, and one of the most overlooked complications is diabetic autonomic neuropathy (DAN). This condition affects the autonomic nervous system, which controls various involuntary functions of the body, such as heart rate, blood pressure, digestion, and bowel movements. DAN can cause a wide range of symptoms, from mild to severe, and can significantly impact a person’s quality of life. In this article, we will delve into the world of diabetic autonomic neuropathy, exploring its causes, symptoms, diagnosis, and most importantly, management strategies to help you take control of your condition.
Understanding Diabetic Autonomic Neuropathy
Diabetic autonomic neuropathy is a type of nerve damage that occurs when high blood sugar levels damage the autonomic nervous system. This system is responsible for regulating various bodily functions, including:
- Heart rate and blood pressure
- Digestion and bowel movements
- Bladder function
- Sweat production
- Pupil response
- Sexual function
When the autonomic nerves are damaged, these functions can become disrupted, leading to a range of symptoms.
Causes and Risk Factors
The primary cause of diabetic autonomic neuropathy is prolonged exposure to high blood sugar levels. However, several other factors can increase the risk of developing DAN, including:
- Duration of diabetes: The longer you have diabetes, the higher the risk of developing DAN.
- Poor blood sugar control: High blood sugar levels can damage the nerves over time.
- Age: Older adults are more likely to develop DAN.
- Other health conditions: Certain health conditions, such as high blood pressure, high cholesterol, and obesity, can increase the risk of developing DAN.
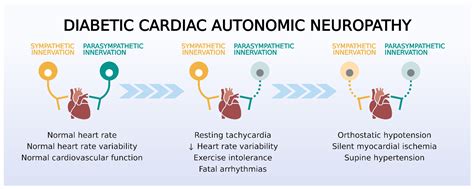
Symptoms of Diabetic Autonomic Neuropathy
The symptoms of diabetic autonomic neuropathy can vary depending on the specific nerves affected. Some common symptoms include:
- Orthostatic hypotension: A sudden drop in blood pressure when standing up, leading to dizziness, lightheadedness, or fainting.
- Gastroparesis: Delayed stomach emptying, leading to nausea, vomiting, bloating, and abdominal pain.
- Urinary retention: Difficulty emptying the bladder, leading to frequent urination, urinary tract infections, or incontinence.
- Constipation: Slowed bowel movements, leading to infrequent bowel movements, straining during bowel movements, or hard stools.
- Sweating abnormalities: Excessive sweating or decreased sweating, leading to heat intolerance or cold intolerance.
- Sexual dysfunction: Erectile dysfunction, vaginal dryness, or decreased libido.
Diagnosis of Diabetic Autonomic Neuropathy
Diagnosing diabetic autonomic neuropathy can be challenging, as the symptoms can be similar to those of other conditions. A comprehensive medical evaluation, including a physical exam, medical history, and laboratory tests, is necessary to diagnose DAN. Some common diagnostic tests include:
- Autonomic function tests: These tests measure the function of the autonomic nervous system, including heart rate variability and blood pressure response to standing.
- Electromyography (EMG): This test measures the electrical activity of muscles to assess nerve damage.
- Nerve conduction studies: These tests measure the speed and strength of electrical signals in nerves.
Management Strategies
While there is no cure for diabetic autonomic neuropathy, various management strategies can help alleviate symptoms and improve quality of life. These include:
- Blood sugar control: Maintaining good blood sugar control through medication, diet, and exercise can help slow the progression of nerve damage.
- Medications: Certain medications, such as fludrocortisone, midodrine, and pyridostigmine, can help manage specific symptoms, such as orthostatic hypotension and gastroparesis.
- Lifestyle modifications: Making healthy lifestyle choices, such as exercising regularly, eating a balanced diet, and managing stress, can help improve overall health and reduce symptoms.
- Alternative therapies: Alternative therapies, such as acupuncture, yoga, and meditation, may help alleviate symptoms and improve quality of life.
What are the most common symptoms of diabetic autonomic neuropathy?
+The most common symptoms of diabetic autonomic neuropathy include orthostatic hypotension, gastroparesis, urinary retention, constipation, sweating abnormalities, and sexual dysfunction.
How is diabetic autonomic neuropathy diagnosed?
+Diabetic autonomic neuropathy is diagnosed through a comprehensive medical evaluation, including a physical exam, medical history, and laboratory tests, such as autonomic function tests, electromyography, and nerve conduction studies.
Can diabetic autonomic neuropathy be prevented?
+While diabetic autonomic neuropathy cannot be completely prevented, maintaining good blood sugar control through medication, diet, and exercise can help slow the progression of nerve damage and reduce the risk of developing DAN.
In conclusion, diabetic autonomic neuropathy is a complex condition that requires a comprehensive management approach. By understanding the causes, symptoms, diagnosis, and management strategies, individuals with diabetes can take control of their condition and improve their quality of life. It is essential to work closely with healthcare providers to develop a personalized management plan that addresses specific symptoms and needs. With the right approach, it is possible to alleviate symptoms, slow the progression of nerve damage, and improve overall health and well-being.



