Enhanced Recovery After Surgery
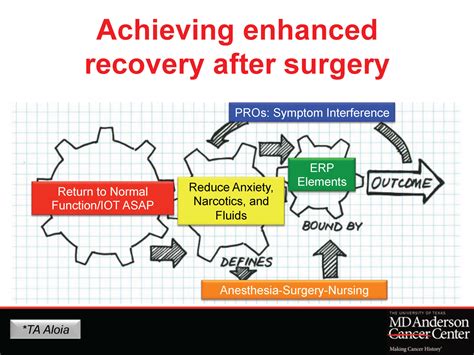
The concept of Enhanced Recovery After Surgery (ERAS) has revolutionized the way surgeons, anesthesiologists, and other healthcare professionals approach patient care in the perioperative period. By implementing evidence-based protocols and multidisciplinary teamwork, ERAS aims to minimize the stress response to surgery, reduce complications, and accelerate recovery. This comprehensive approach has been shown to improve patient outcomes, reduce hospital stays, and decrease healthcare costs.
Historical Evolution of ERAS
The idea of ERAS originated in the 1990s, when a group of surgeons and anesthesiologists in Europe began exploring ways to optimize postoperative care. They recognized that traditional surgical practices, such as prolonged fasting and bed rest, were not based on scientific evidence and could actually hinder recovery. Through a series of studies and clinical trials, the ERAS protocol was developed and refined, incorporating elements such as preoperative education, optimized fluid management, and early mobilization.
Key Components of ERAS
ERAS involves a multidisciplinary approach, with various healthcare professionals working together to implement a range of evidence-based interventions. Some of the key components of ERAS include:
- Preoperative optimization: Patients undergo thorough preoperative evaluations, including medical history, physical examination, and laboratory tests, to identify potential risks and optimize their condition before surgery.
- Fluid management: Intraoperative and postoperative fluid management is carefully controlled to minimize fluid overload and reduce the risk of complications.
- Pain management: Multimodal pain management strategies are used to minimize opioid use and reduce postoperative pain.
- Early mobilization: Patients are encouraged to get out of bed and mobilize as soon as possible after surgery to reduce the risk of complications, such as deep vein thrombosis and pneumonia.
- Nutritional support: Patients receive early nutritional support, including oral nutrition or enteral feeding, to promote wound healing and reduce the risk of malnutrition.
Benefits of ERAS
The benefits of ERAS are numerous and well-documented. Some of the most significant advantages include:
- Reduced hospital stays: ERAS has been shown to reduce hospital stays by up to 30%, resulting in significant cost savings and improved patient satisfaction.
- Decreased complications: ERAS has been associated with a reduction in postoperative complications, such as wound infections, respiratory problems, and cardiopulmonary events.
- Improved pain management: ERAS protocols have been shown to reduce postoperative pain and minimize opioid use, resulting in improved patient comfort and reduced risk of addiction.
- Enhanced patient satisfaction: ERAS has been associated with improved patient satisfaction, as patients are more likely to feel empowered and involved in their care.
Implementation of ERAS
Implementing ERAS requires a multidisciplinary approach, with collaboration between surgeons, anesthesiologists, nurses, and other healthcare professionals. Some of the key steps involved in implementing ERAS include:
- Developing a protocol: A multidisciplinary team develops a comprehensive ERAS protocol, incorporating evidence-based interventions and guidelines.
- Educating staff: All healthcare staff involved in patient care are educated on the ERAS protocol and their roles and responsibilities.
- Monitoring and evaluation: Patient outcomes are closely monitored and evaluated, with ongoing adjustments made to the ERAS protocol as needed.
Challenges and Limitations
While ERAS has been shown to be highly effective, there are some challenges and limitations to its implementation. Some of the key challenges include:
- Resistance to change: Some healthcare professionals may be resistant to changing traditional practices and adopting new protocols.
- Limited resources: Implementing ERAS may require significant resources, including staff education and training, new equipment, and changes to hospital infrastructure.
- Variability in patient populations: ERAS protocols may need to be adapted to accommodate variability in patient populations, such as older adults or those with comorbidities.
Future Directions
As ERAS continues to evolve, there are several future directions that hold promise for improving patient outcomes and reducing healthcare costs. Some of the key areas of focus include:
- Personalized medicine: ERAS protocols may be tailored to individual patient needs, incorporating genetic profiling and other advanced technologies.
- Telemedicine: Telemedicine may be used to extend ERAS protocols to remote or underserved populations, improving access to care and reducing healthcare disparities.
- Artificial intelligence: Artificial intelligence may be used to analyze large datasets and identify patterns and predictors of postoperative complications, allowing for more targeted interventions and improved patient outcomes.
What are the key benefits of Enhanced Recovery After Surgery (ERAS) protocols?
+The key benefits of ERAS protocols include reduced hospital stays, decreased complications, improved pain management, and enhanced patient satisfaction.
How are ERAS protocols implemented in clinical practice?
+ERAS protocols are implemented through a multidisciplinary approach, involving collaboration between surgeons, anesthesiologists, nurses, and other healthcare professionals. This includes developing a protocol, educating staff, and monitoring and evaluating patient outcomes.
What are some of the challenges and limitations of ERAS protocols?
+Some of the challenges and limitations of ERAS protocols include resistance to change, limited resources, and variability in patient populations. These challenges may require adaptations to the ERAS protocol and ongoing evaluation and improvement.
In conclusion, Enhanced Recovery After Surgery (ERAS) protocols have revolutionized the way healthcare professionals approach patient care in the perioperative period. By implementing evidence-based interventions and multidisciplinary teamwork, ERAS has been shown to improve patient outcomes, reduce hospital stays, and decrease healthcare costs. As ERAS continues to evolve, it is likely to play an increasingly important role in shaping the future of surgical care.


