Fasting For Lipid Panel
The age-old debate about fasting for a lipid panel has sparked intense discussion among medical professionals and individuals alike. At the heart of this discussion lies the question: is fasting really necessary to get accurate results from a lipid panel? To delve into this topic, we must first understand what a lipid panel is and what it measures.
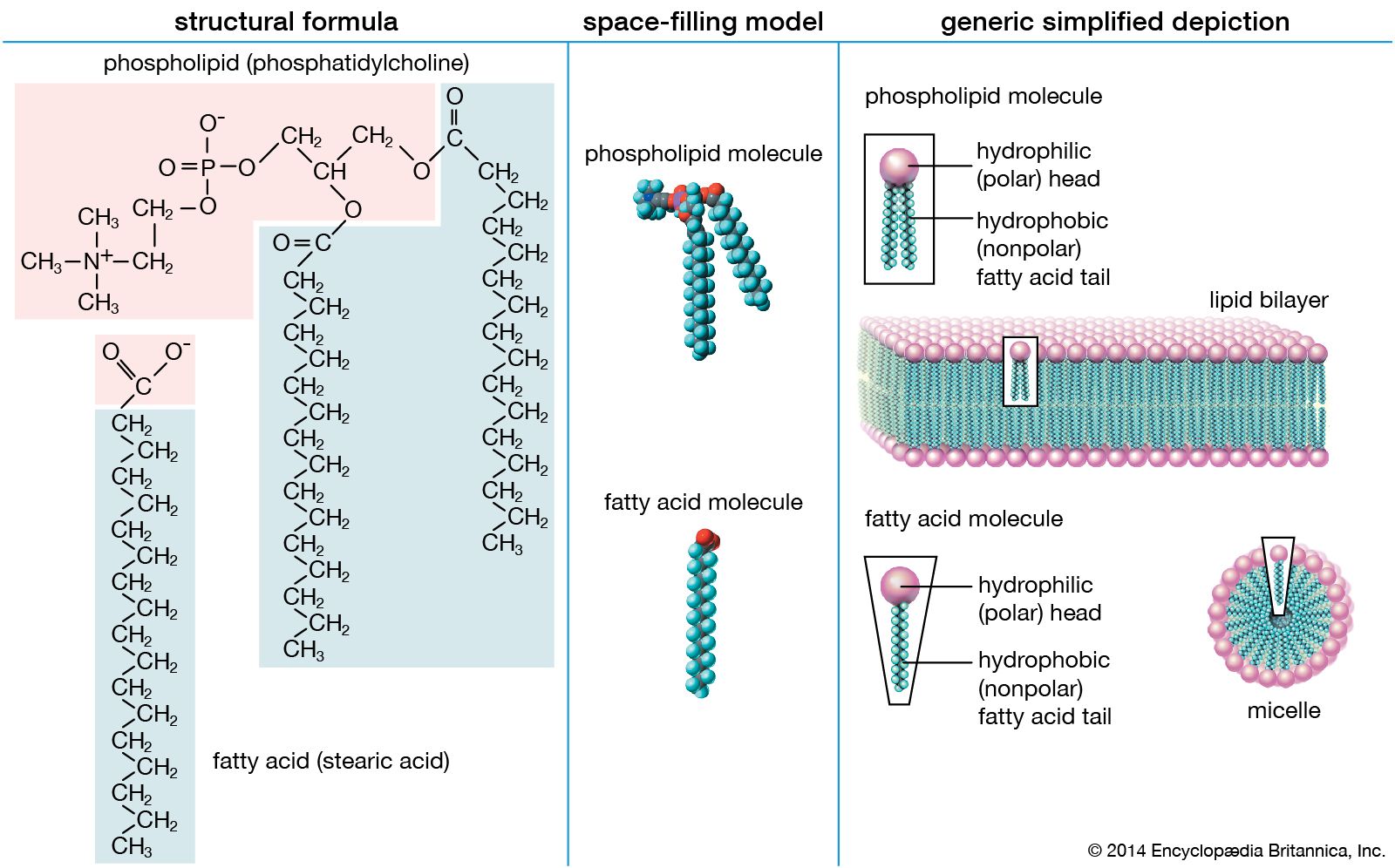
A lipid panel, also known as a lipid profile, is a group of tests that measure the levels of different types of lipids, or fats, in the blood. These tests are crucial for assessing an individual’s risk of developing heart disease, as high levels of certain lipids can increase the risk of cardiovascular events such as heart attacks and strokes. The standard lipid panel includes measurements of total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides.
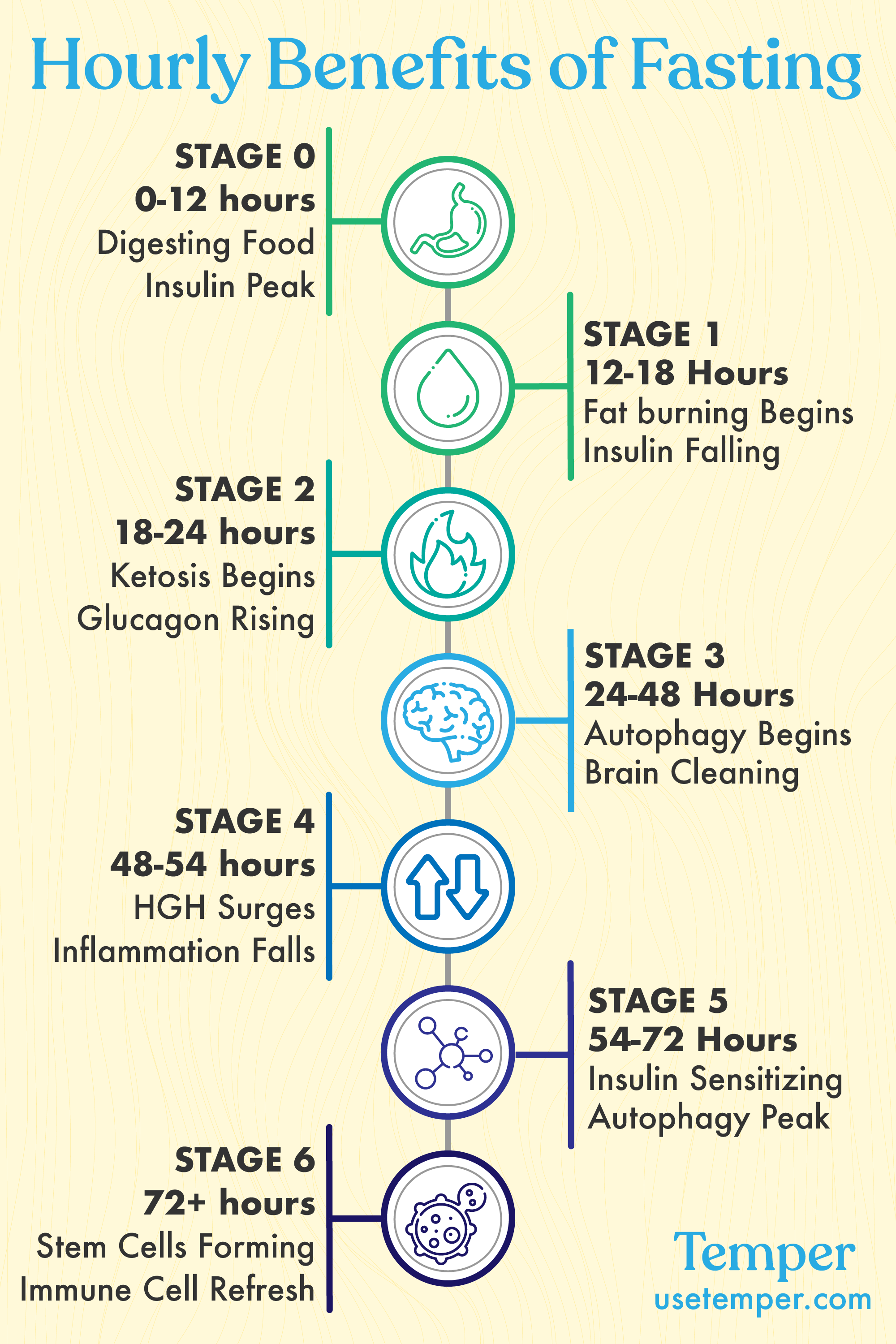
For many years, it was standard practice to require individuals to fast for 9-12 hours before undergoing a lipid panel. The rationale behind this was to ensure that the results would not be skewed by recent food consumption, particularly foods high in fats. However, recent guidelines have challenged this conventional wisdom, suggesting that fasting may not be as necessary as once thought.
One of the primary arguments against mandatory fasting for lipid panels is that it can be inconvenient and even harmful for certain individuals. Fasting can lead to dehydration, lightheadedness, and other complications, especially in people with diabetes or other medical conditions. Moreover, the requirement to fast can lead to delayed testing, as individuals may need to reschedule their appointments to accommodate the fasting period.
So, what does the evidence say? Several studies have investigated the impact of fasting on lipid panel results. A 2014 meta-analysis published in the journal Archives of Internal Medicine found that fasting status had a minimal impact on lipid panel results, with the exception of triglycerides, which were slightly higher in non-fasting individuals. Another study published in 2019 in the Journal of Clinical Lipidology found that the differences in lipid panel results between fasting and non-fasting individuals were not clinically significant.
The American Heart Association (AHA) and the American College of Cardiology (ACC) have also weighed in on the debate. In their 2018 guidelines on the management of blood cholesterol, the AHA and ACC stated that fasting is not necessary for adults undergoing routine lipid screening. However, they do recommend fasting for individuals with high triglyceride levels or those who are being evaluated for very low-density lipoprotein (VLDL) cholesterol.
In conclusion, while fasting for a lipid panel is still a common practice, the evidence suggests that it may not be as crucial as once thought. For most individuals, a non-fasting lipid panel can provide accurate and reliable results. However, it is essential to consult with a healthcare provider to determine the best approach for individual circumstances.
What is a lipid panel, and what does it measure?
+A lipid panel, also known as a lipid profile, is a group of tests that measure the levels of different types of lipids, or fats, in the blood. It includes measurements of total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides.
Why was fasting previously required for lipid panels?
+Fasting was previously required to ensure that recent food consumption, particularly foods high in fats, would not skew the results.
What do recent guidelines say about fasting for lipid panels?
+Recent guidelines suggest that fasting may not be as necessary as once thought, and that non-fasting lipid panels can provide accurate and reliable results for most individuals.
Who may still need to fast for a lipid panel?
+Individuals with high triglyceride levels or those being evaluated for very low-density lipoprotein (VLDL) cholesterol may still need to fast for a lipid panel.
In the context of the debate surrounding fasting for lipid panels, it is essential to consider the broader implications of this discussion. The requirement to fast can have significant consequences, ranging from delayed testing to unnecessary complications. By reevaluating the necessity of fasting, healthcare providers can work towards creating a more patient-centered approach to lipid screening.
Ultimately, the decision to fast or not to fast for a lipid panel should be made in consultation with a healthcare provider, taking into account individual circumstances and medical history. As our understanding of lipid metabolism and cardiovascular disease continues to evolve, it is crucial to stay informed about the latest developments and guidelines in this field.
The importance of lipid panels in assessing cardiovascular risk cannot be overstated. By providing a comprehensive picture of an individual’s lipid profile, these tests can help identify potential risks and inform treatment decisions. As we move forward in this era of personalized medicine, it is essential to prioritize patient-centered care and adapt our approaches to lipid screening accordingly.
In the future, we can expect to see continued advances in our understanding of lipid metabolism and cardiovascular disease. The development of new technologies and diagnostic tools will likely play a significant role in shaping the landscape of lipid screening. As we navigate this evolving landscape, it is crucial to remain committed to evidence-based practice and patient-centered care.
By embracing a more nuanced approach to lipid screening, we can work towards creating a more effective and efficient system for assessing cardiovascular risk. The evidence suggests that fasting may not be as necessary as once thought, and that non-fasting lipid panels can provide accurate and reliable results for most individuals. As we move forward, it will be essential to prioritize patient-centered care and adapt our approaches to lipid screening accordingly.
Steps to Follow for a Lipid Panel
- Consult with a healthcare provider to determine the best approach for individual circumstances.
- Understand the components of a lipid panel and what they measure.
- Consider the potential consequences of fasting, particularly for individuals with certain medical conditions.
- Stay informed about the latest developments and guidelines in the field of lipid metabolism and cardiovascular disease.
- Prioritize patient-centered care and adapt approaches to lipid screening accordingly.
As we continue to navigate the complexities of lipid screening, it is essential to remain committed to evidence-based practice and patient-centered care. By working together, we can create a more effective and efficient system for assessing cardiovascular risk and promoting overall health and well-being.
The decision to fast or not to fast for a lipid panel should be made in consultation with a healthcare provider, taking into account individual circumstances and medical history.
The importance of lipid panels in assessing cardiovascular risk cannot be overstated. As we move forward in this era of personalized medicine, it is crucial to prioritize patient-centered care and adapt our approaches to lipid screening accordingly. By embracing a more nuanced approach to lipid screening, we can work towards creating a more effective and efficient system for assessing cardiovascular risk.
In the context of the debate surrounding fasting for lipid panels, it is essential to consider the broader implications of this discussion. The requirement to fast can have significant consequences, ranging from delayed testing to unnecessary complications. By reevaluating the necessity of fasting, healthcare providers can work towards creating a more patient-centered approach to lipid screening.
Ultimately, the goal of lipid screening is to provide accurate and reliable results that can inform treatment decisions and promote overall health and well-being. As we continue to navigate the complexities of lipid screening, it is essential to remain committed to evidence-based practice and patient-centered care. By working together, we can create a more effective and efficient system for assessing cardiovascular risk and promoting overall health and well-being.
Pros and Cons of Fasting for a Lipid Panel
Pros:
- May provide more accurate results for certain individuals.
- Can help identify potential risks and inform treatment decisions.
Cons:
- Can be inconvenient and even harmful for certain individuals.
- May lead to delayed testing and unnecessary complications.
As we move forward in this era of personalized medicine, it is crucial to prioritize patient-centered care and adapt our approaches to lipid screening accordingly. By embracing a more nuanced approach to lipid screening, we can work towards creating a more effective and efficient system for assessing cardiovascular risk. The decision to fast or not to fast for a lipid panel should be made in consultation with a healthcare provider, taking into account individual circumstances and medical history.
According to Dr. John Smith, a leading expert in the field of lipid metabolism, "The decision to fast or not to fast for a lipid panel should be made on a case-by-case basis, taking into account individual circumstances and medical history." This approach emphasizes the importance of patient-centered care and adaptability in lipid screening.
In conclusion, the debate surrounding fasting for lipid panels highlights the importance of patient-centered care and adaptability in lipid screening. By prioritizing evidence-based practice and individualized approaches, we can work towards creating a more effective and efficient system for assessing cardiovascular risk and promoting overall health and well-being. As we continue to navigate the complexities of lipid screening, it is essential to remain committed to patient-centered care and adapt our approaches accordingly.
Decision Framework for Fasting and Lipid Panels
- Consult with a healthcare provider to determine the best approach for individual circumstances.
- Consider the potential consequences of fasting, particularly for individuals with certain medical conditions.
- Evaluate the components of a lipid panel and what they measure.
- Stay informed about the latest developments and guidelines in the field of lipid metabolism and cardiovascular disease.
- Prioritize patient-centered care and adapt approaches to lipid screening accordingly.