Hemoglobin A1c Test
The Hemoglobin A1c (HbA1c) test has become a cornerstone in the diagnosis and management of diabetes, offering a snapshot of an individual’s average blood glucose levels over the preceding 2-3 months. This crucial measurement is derived from a simple blood test that detects the amount of glucose that has bound to hemoglobin in red blood cells. The significance of the HbA1c test lies in its ability to provide healthcare providers with a clear picture of how well diabetes is being managed, guiding treatment decisions to ensure optimal glucose control and minimize the risk of diabetes-related complications.
Understanding Hemoglobin A1c
Hemoglobin is a protein in red blood cells that carries oxygen throughout the body. When glucose is present in the blood, some of it binds to hemoglobin, forming glycosylated hemoglobin, or HbA1c. The higher the blood glucose levels, the more glucose binds to hemoglobin. Since red blood cells have a lifespan of approximately 120 days, measuring HbA1c levels gives an estimate of the average blood glucose levels over the past 2-3 months. This is particularly useful for individuals with diabetes, as it helps in assessing the effectiveness of their treatment plan and making necessary adjustments.
The Significance of HbA1c Levels
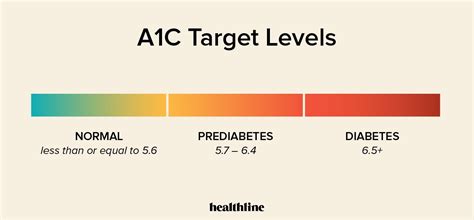
The interpretation of HbA1c levels is pivotal in diabetes care. For individuals without diabetes, a normal HbA1c level is typically below 5.7%. For those with diabetes, the American Diabetes Association recommends an HbA1c goal of less than 7% for most adults, though this target may vary depending on individual characteristics, such as age, duration of diabetes, life expectancy, resources, and support system. Achieving and maintaining this goal is crucial, as elevated HbA1c levels are associated with an increased risk of diabetic complications, including cardiovascular diseases, kidney disease, and nerve damage.
How the HbA1c Test is Performed
The HbA1c test is straightforward and involves a single blood sample, usually drawn from a vein in the arm. The blood is then sent to a laboratory for analysis. In some cases, point-of-care devices may be used to provide immediate results. The test does not require fasting or any special preparation, making it convenient for patients. However, it’s essential to note that certain conditions, such as recent blood transfusions, hemoglobinopathies (e.g., sickle cell disease), and severe kidney or liver disease, may affect the accuracy of the HbA1c test, requiring alternative methods of assessing glucose control.
Limitations and Considerations
While the HbA1c test is invaluable for monitoring long-term glucose control, it has its limitations. For example, it may not accurately reflect glucose levels in individuals with disorders that affect red blood cell turnover, such as hemolytic anemia. Additionally, HbA1c does not provide information on daily glucose fluctuations or hypoglycemic episodes, making continuous glucose monitoring (CGM) or self-monitoring of blood glucose (SMBG) complementary tools in diabetes management. Furthermore, achieving an HbA1c target does not solely define successful diabetes management; considerations such as blood pressure control, lipid management, and lifestyle interventions are also critical.
Managing Diabetes with HbA1c Insights
For individuals living with diabetes, understanding their HbA1c results is key to making informed decisions about their care. If HbA1c levels are higher than the target, it may indicate the need for adjustments in medication, diet, or physical activity. Conversely, achieving or maintaining target HbA1c levels suggests that the current management plan is effective. Healthcare providers use HbA1c results in conjunction with other clinical information to tailor treatment plans, emphasizing the importance of ongoing monitoring and flexible management strategies.
Future Perspectives and Emerging Technologies
The landscape of diabetes management is evolving, with advancements in technology and a deeper understanding of the disease’s pathophysiology. Emerging technologies, such as more sophisticated CGM systems and insulin pumps with predictive analytics, are enhancing the precision of glucose control. Moreover, research into new therapeutic agents and personalized medicine approaches aims to further tailor diabetes treatment to individual patient profiles, potentially leading to improved outcomes and enhanced quality of life for those affected by diabetes.
Conclusion
The Hemoglobin A1c test stands as a vital tool in the management of diabetes, offering a window into the effectiveness of current treatment strategies and guiding adjustments to achieve optimal glucose control. As our understanding of diabetes and its complexities deepens, the integration of HbA1c testing with other monitoring technologies and therapeutic innovations promises to improve patient outcomes, mitigating the risk of diabetes-related complications and enhancing the well-being of individuals worldwide affected by this condition.
What does an HbA1c level of 7% mean for a person with diabetes?
+An HbA1c level of 7% indicates that, on average, blood glucose levels have been well-controlled over the past 2-3 months, meeting the general target recommended for most adults with diabetes. However, individual targets may vary based on specific health circumstances and guidelines.
Can the HbA1c test be used for diagnosing diabetes?
+Yes, the HbA1c test can be used as a diagnostic tool for diabetes. An HbA1c level of 6.5% or higher is indicative of diabetes, according to the American Diabetes Association and other international guidelines. However, diagnosis should be confirmed with repeat testing on a different day, unless symptoms of hyperglycemia or hyperglycemic crisis are present.
How often should the HbA1c test be performed for someone with established diabetes?
+The frequency of HbA1c testing in individuals with established diabetes depends on the stability of their condition and the effectiveness of their treatment plan. Generally, HbA1c levels should be checked at least twice a year in patients who are meeting treatment goals and have stable glycemic control. More frequent testing (every 3 months) is recommended for individuals whose therapy has changed or whose glucose control is not optimal.
Are there any conditions that can affect HbA1c test results?
+Yes, several conditions can affect HbA1c test results. These include recent blood transfusions, hemoglobinopathies (like sickle cell disease), severe kidney or liver disease, and certain anemias. In such cases, alternative methods for assessing glucose control may be necessary.
How does lifestyle impact HbA1c levels?
+Lifestyle factors, including diet, physical activity, and smoking status, significantly impact HbA1c levels. Adhering to a balanced diet low in added sugars and saturated fats, engaging in regular physical activity, maintaining a healthy weight, and avoiding tobacco can help in achieving and maintaining target HbA1c levels.