How Does Lidocaine Work
Lidocaine, a local anesthetic and antiarrhythmic drug, has been a cornerstone in medical practice for decades, particularly in the realm of pain management and cardiac care. Its mechanism of action, while complex, can be simplified to understand its effectiveness and widespread application. To delve into how lidocaine works, it’s essential to first grasp the basics of its pharmacological properties and then explore its effects on the body.
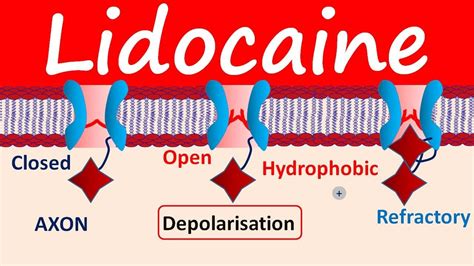
At its core, lidocaine belongs to the class of drugs known as amide local anesthetics. It functions by inhibiting the influx of sodium ions into nerve cells, which is crucial for the initiation and propagation of nerve impulses. Normally, when a nerve is stimulated, voltage-gated sodium channels open, allowing sodium ions to rush into the cell. This influx of positive ions depolarizes the nerve cell membrane, leading to the generation of an action potential that travels along the length of the nerve fiber. Lidocaine, when applied locally or administered systemically, penetrates the nerve cell membrane in its uncharged form and then binds to the sodium channels from the inside, stabilizing them in an inactive state. This binding blocks the influx of sodium ions, thereby preventing depolarization of the nerve cell and the subsequent generation of an action potential.
The effect of lidocaine on sodium channels is not only limited to sensory nerves but also extends to motor nerves, which is why it can cause muscle weakness when administered in higher doses or closer to the site of motor nerve function. However, its primary clinical use as a local anesthetic capitalizes on its ability to reversibly block sensory nerve conduction, providing relief from pain without causing permanent damage to the nerves.
In addition to its local anesthetic effects, lidocaine also possesses antiarrhythmic properties, particularly for the treatment of ventricular arrhythmias. In the context of cardiac tissue, lidocaine works by reducing automaticity and increasing the threshold for electrical excitability. It does so by blocking sodium channels in the heart, which helps in stabilizing the cardiac membrane and reducing the likelihood of aberrant rhythms. This is especially useful in the acute management of ventricular tachycardia or fibrillation, where rapid control of the heart rhythm is critical.
The pharmacokinetics of lidocaine, including its absorption, distribution, metabolism, and excretion, play a significant role in its effectiveness and safety profile. When administered locally, lidocaine is absorbed systemically to varying degrees depending on the site of administration, the dose used, and the presence of vasoconstrictors like epinephrine, which can reduce systemic absorption and prolong local action. Systemically, lidocaine undergoes extensive first-pass metabolism in the liver, where it is primarily metabolized by the hepatic cytochrome P450 enzymes into monoethylglycinexylidide (MEGX) and then to glycinexylidide (GX), both of which retain some pharmacological activity.
Despite its utility, the use of lidocaine is not without risks. Systemic toxicity, particularly to the central nervous and cardiovascular systems, can occur if plasma concentrations of lidocaine exceed therapeutic levels. Early signs of toxicity may include perioral numbness, metallic taste, and dizziness, progressing to seizures and coma in severe cases. Cardiac manifestations can range from mild changes in heart rate and rhythm to profound effects such as decreased cardiac contractility and, in extreme cases, cardiac arrest.
In conclusion, lidocaine’s multifaceted role in both local anesthesia and antiarrhythmic therapy stems from its ability to modulate ion channel function in nerve and cardiac tissues. Its effectiveness in providing pain relief and stabilizing aberrant heart rhythms has solidified its position as a fundamental component of pharmacological interventions in clinical practice. Nonetheless, its use must be carefully managed to avoid toxicity, underscoring the importance of a comprehensive understanding of its pharmacodynamics and pharmacokinetics.
FAQ Section
What are the primary uses of lidocaine in medical practice?
+Lidocaine is primarily used as a local anesthetic to provide pain relief and as an antiarrhythmic drug to manage certain types of irregular heart rhythms, particularly ventricular arrhythmias.
How does lidocaine work to block pain signals?
+Lidocaine works by penetrating the nerve cell membrane and binding to sodium channels from the inside, which blocks the influx of sodium ions necessary for the generation of an action potential. This prevents the depolarization of the nerve cell and thus stops the transmission of pain signals.
What are the risks of using lidocaine, and how can toxicity be prevented?
+The risks of using lidocaine include systemic toxicity affecting the central nervous and cardiovascular systems. Toxicity can be prevented by carefully managing the dose, selecting the appropriate route of administration, and monitoring patients closely for early signs of toxicity. Adherence to recommended dosages and awareness of factors that may alter lidocaine’s pharmacokinetics, such as liver dysfunction, are also crucial.
Can lidocaine be used in all types of arrhythmias?
+Lidocaine is specifically useful for treating ventricular arrhythmias, such as ventricular tachycardia and ventricular fibrillation. It is not typically used for supraventricular arrhythmias, as other antiarrhythmic drugs or interventions may be more appropriate for these conditions.
How long does lidocaine stay in the system after administration?
+The duration of action of lidocaine depends on the route of administration and the presence of any factors that may alter its metabolism and excretion. Locally administered lidocaine can provide relief from pain for several hours, while systemically administered lidocaine for arrhythmia management may have effects that last as long as the drug and its active metabolites remain in the system, typically several hours.