How Is Gfr Calculated
Glomerular filtration rate (GFR) is a crucial measure of kidney function, representing the volume of fluid filtered from the renal glomerular capillaries into the Bowman’s capsule per unit time. Calculating GFR is essential for diagnosing and monitoring kidney disease, as it provides valuable insights into the kidneys’ ability to filter waste products from the blood. There are several methods to calculate GFR, each with its own advantages and limitations.
1. Serum Creatinine-based Calculations
The most common method for estimating GFR (eGFR) in clinical practice involves using serum creatinine levels, along with other variables such as age, sex, and race. The two most widely used equations are the Modification of Diet in Renal Disease (MDRD) study equation and the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.
MDRD Study Equation: [ \text{eGFR (mL/min/1.73 m^2)} = 186 \times (\text{serum creatinine})^{-1.154} \times (\text{age})^{-0.203} \times (0.742 \text{ if female}) \times (1.212 \text{ if African American}) ]
CKD-EPI Equation: For females: [ \text{eGFR (mL/min/1.73 m^2)} = 144 \times (\text{serum creatinine})^{-0.329} \times (0.993)^{\text{age}} \times 0.659 ] For males: [ \text{eGFR (mL/min/1.73 m^2)} = 141 \times (\text{serum creatinine})^{-0.411} \times (0.993)^{\text{age}} ]
Adjustments for African Americans are made by multiplying the result by 1.159.
2. Cystatin C-based Calculations
Cystatin C, a protein produced by all cells, is filtered by the kidneys and can serve as an alternative to serum creatinine for estimating GFR, especially in situations where creatinine levels may not accurately reflect kidney function, such as in muscle-wasting diseases.
- CKD-EPI Cystatin C Equation: [ \text{eGFR (mL/min/1.73 m^2)} = 133 \times (\text{cystatin C})^{-0.499} \times (0.996)^{\text{age}} \times (0.932 \text{ if female}) ]
3. Combination of Creatinine and Cystatin C
Using both serum creatinine and cystatin C can provide a more accurate estimation of GFR than either marker alone, particularly in certain populations or clinical scenarios.
- CKD-EPI Creatinine-Cystatin C Equation: [ \text{eGFR (mL/min/1.73 m^2)} = 135 \times (\text{creatinine})^{-0.207} \times (\text{cystatin C})^{-0.601} \times (0.995)^{\text{age}} \times (0.969 \text{ if female}) \times (1.08 \text{ if African American}) ]
4. Direct Measurement of GFR
While estimating GFR through equations is common, direct measurement involves injecting a substance that is completely filtered by the kidneys and then measuring its clearance from the blood. This can be done with substances like inulin, iothalamate, or chromium-51 ethylenediaminetetraacetic acid (EDTA). However, due to the complexity, cost, and invasiveness of these procedures, they are typically reserved for research or specific clinical situations where highly accurate measurements are necessary.
Clinical Interpretation
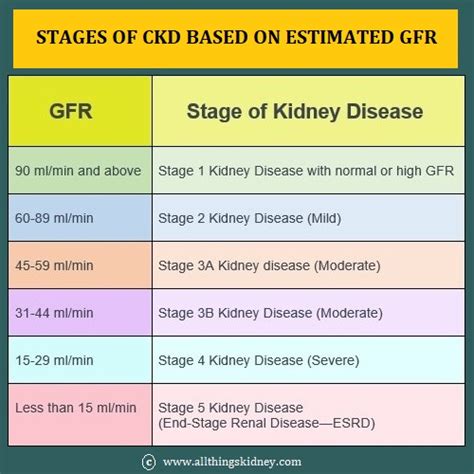
Understanding the GFR calculation is crucial for clinical interpretation. GFR values are categorized into stages of kidney disease:
- Stage 1: Kidney damage with normal or increased GFR (>90 mL/min/1.73 m^2)
- Stage 2: Mild kidney disease (60-89 mL/min/1.73 m^2)
- Stage 3: Moderate kidney disease, further divided into 3A (45-59 mL/min/1.73 m^2) and 3B (30-44 mL/min/1.73 m^2)
- Stage 4: Severe kidney disease (15-29 mL/min/1.73 m^2)
- Stage 5: Kidney failure (<15 mL/min/1.73 m^2 or on dialysis)
Each calculation method has its strengths and weaknesses, and the choice often depends on the clinical scenario, the availability of data, and the patient’s characteristics. Accurate calculation and interpretation of GFR are vital for managing patients with kidney disease, making informed decisions about the initiation of renal replacement therapy, and monitoring the progression of kidney disease over time.
Frequently Asked Questions
What is the primary use of calculating GFR in clinical practice?
+The primary use of calculating GFR is to assess kidney function. It helps in diagnosing kidney disease, monitoring its progression, and making decisions about the need for dialysis or kidney transplantation.
Which formula is more accurate for estimating GFR, MDRD or CKD-EPI?
+The CKD-EPI equation is generally considered more accurate than the MDRD equation, especially at higher levels of GFR. It is less biased and provides a more accurate estimation across different populations and GFR ranges.