Hysteroscopy Dilation And Curettage
Hysteroscopy dilation and curettage (D&C) is a medical procedure that combines two distinct techniques to diagnose and treat abnormalities within the uterus. The procedure is typically performed by a gynecologist or a specialist in reproductive health and involves the use of a hysteroscope, a thin, flexible or rigid telescope-like instrument, to visually examine the inside of the uterus. This visualization is then followed by a dilation and curettage procedure, where the cervix is dilated, and a curette, a spoon-shaped instrument, is used to remove tissue from the uterus.
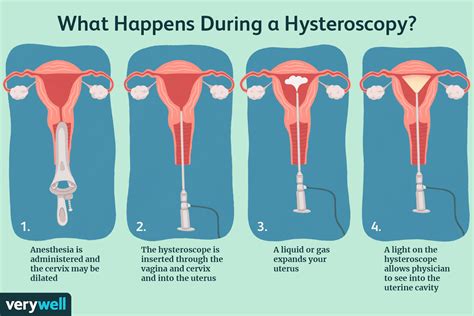
Understanding the Procedure
The hysteroscopy aspect of the procedure allows for a detailed examination of the uterine cavity. The hysteroscope is inserted through the cervix and into the uterus, and it transmits images to a monitor for the doctor to view. This part of the procedure can help identify abnormalities such as fibroids, polyps, and other structural issues within the uterus.
Following the diagnostic phase, if necessary, the procedure moves on to the dilation and curettage (D&C) part. The cervix is gently dilated to allow for the insertion of the curette. The curette is then used to gently scrape away the lining of the uterus (endometrium) and remove any abnormal tissue that was identified during the hysteroscopy. This tissue is then sent to a laboratory for further examination under a microscope.
Reasons for the Procedure
There are several reasons why a healthcare provider might recommend a hysteroscopy D&C. These include:
- Abnormal Uterine Bleeding: This is one of the most common reasons for the procedure. If a woman is experiencing unusually heavy, prolonged, or irregular menstrual bleeding, a hysteroscopy D&C can help identify and possibly treat the cause, such as removing polyps or fibroids that may be contributing to the bleeding.
- Investigation of Infertility or Recurrent Miscarriage: In some cases, abnormalities within the uterus can contribute to difficulties in conceiving or maintaining a pregnancy. A hysteroscopy D&C can help identify and sometimes correct these issues.
- Removal of Polyps or Fibroids: These growths can cause a range of symptoms, including abnormal bleeding, and can be removed during a hysteroscopy D&C.
- Removal of Adhesions: Asherman’s syndrome, a condition characterized by the formation of adhesions or scar tissue in the uterus, can be treated with a hysteroscopy D&C.
Preparation and Recovery
Preparation for a hysteroscopy D&C typically involves a series of steps to ensure the patient’s comfort and safety. This may include avoiding food and drink for a certain period before the procedure, stopping certain medications, and arranging for someone to drive the patient home afterward.
The recovery from a hysteroscopy D&C is generally straightforward for most women. Some may experience mild cramping, similar to menstrual cramps, and light bleeding or spotting. These symptoms are usually temporary and can be managed with over-the-counter pain relievers. It’s essential to follow the healthcare provider’s instructions regarding rest, physical activity, and when it’s safe to resume normal activities and sexual intercourse.
Risks and Complications
While hysteroscopy D&C is considered a safe procedure, as with any medical intervention, there are potential risks and complications. These can include:
- Infection: There is a small risk of infection with any invasive procedure.
- Excessive Bleeding: Some women may experience heavier than usual bleeding after the procedure.
- Perforation of the Uterus: Although rare, the instruments used could potentially cause a hole in the uterus.
- Adhesions: The procedure could potentially lead to the formation of adhesions within the uterus.
It’s crucial for patients to discuss these risks and any concerns they may have with their healthcare provider before undergoing the procedure.
Conclusion
Hysteroscopy dilation and curettage is a valuable diagnostic and therapeutic tool for managing a variety of uterine abnormalities. By combining visualization of the uterine cavity with the ability to remove tissue for examination and treat conditions, this procedure offers a comprehensive approach to addressing issues related to abnormal uterine bleeding, infertility, and other uterine conditions. As with any medical procedure, it’s essential to carefully consider the potential benefits and risks and to discuss any questions or concerns with a healthcare provider.
What is the primary purpose of a hysteroscopy D&C procedure?
+The primary purpose is to diagnose and treat abnormalities within the uterus, such as polyps, fibroids, and adhesions, which may cause symptoms like abnormal uterine bleeding or contribute to infertility.
How long does a hysteroscopy D&C procedure typically take?
+The procedure can vary in duration but typically takes between 30 minutes to an hour to complete, depending on the complexity of the case and whether it's performed under local or general anesthesia.
Are there any alternatives to hysteroscopy D&C for treating uterine abnormalities?
+Can a hysteroscopy D&C be performed in an office setting, or is it always done in a hospital?
+While some hysteroscopy procedures can be performed in an office setting under local anesthesia, D&C procedures are often done in an outpatient surgery center or hospital, especially if general anesthesia is planned or if there's a potential for more complex surgery.
In conclusion, while hysteroscopy D&C is a highly effective procedure for diagnosing and treating uterine abnormalities, it’s crucial for patients to be well-informed about what to expect, the potential risks, and the alternatives available. This knowledge empowers them to make informed decisions about their care in consultation with their healthcare provider.



