Iabp Therapy: Comprehensive Support Explained
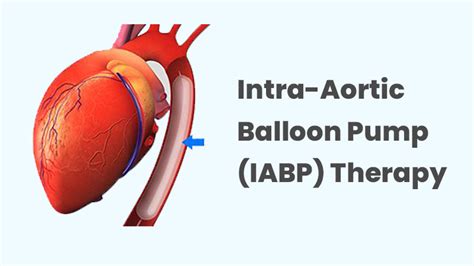
In the realm of cardiovascular medicine, the management of acute myocardial infarction, cardiogenic shock, and other severe cardiac conditions often requires aggressive and supportive therapies. Among these, Intra-Aortic Balloon Pump (IABP) therapy stands out as a crucial intervention that provides circulatory support to the heart. This mechanically assisted therapeutic approach has been pivotal in the management of various cardiac emergencies, offering a bridge to recovery or further definitive treatments for patients in critical need. The purpose of this discussion is to delve into the nuances of IABP therapy, exploring its principles, indications, benefits, and the complexities associated with its implementation.
Historical Evolution of IABP Therapy
The concept of mechanically supporting the heart dates back several decades, with the first IABP being introduced in the 1960s. Since its inception, IABP therapy has undergone significant technological advancements and refinements in clinical application. Initially met with skepticism, it has evolved to become a staple in the arsenal of cardiologists and cardiothoracic surgeons worldwide, particularly in scenarios where pharmacological interventions fall short. The historical evolution of IABP reflects a broader trend in medicine towards the development of more sophisticated and less invasive interventions.
Technical Breakdown: How IABP Works
At its core, an IABP consists of a cylindrical balloon that is placed in the aorta, the body’s largest artery, via a catheter inserted through the femoral artery in the groin. The balloon is synchronized with the patient’s electrocardiogram (ECG) and inflates during diastole (the relaxation phase of the heart), increasing aortic pressure and enhancing coronary perfusion. Simultaneously, it deflates during systole (the contraction phase), reducing afterload and facilitating the heart’s pumping action. This synchronized inflation and deflation significantly augment cardiac output and reduce the workload of the heart, providing critical support during periods of myocardial stress or failure.
Problem-Solution Framework: Clinical Indications for IABP Therapy
IABP therapy is indicated in a variety of clinical scenarios where there is a need for temporary support of the heart’s pumping function. Some of the key indications include:
- Cardiogenic Shock: A condition characterized by inadequate circulation of blood, leading to insufficient delivery of oxygen to vital organs. IABP therapy can help augment cardiac output and improve tissue perfusion.
- Acute Myocardial Infarction (AMI) Complicated by Shock or Severe Ischemia: In instances where AMI is complicated by conditions such as ventricular septal defect or severe mitral regurgitation, IABP can be lifesaving.
- Mechanical Complications of AMI: Conditions such as papillary muscle rupture leading to acute mitral regurgitation can benefit from the temporary support offered by IABP.
- Preoperative and Postoperative Support in High-Risk Cardiac Surgery: Patients undergoing high-risk cardiac surgical procedures may benefit from IABP support to reduce the risk of cardiac complications.
Comparative Analysis: IABP Versus Other Mechanical Support Devices
The landscape of mechanical circulatory support has expanded significantly over the years, with devices such as ventricular assist devices (VADs) and extracorporeal membrane oxygenation (ECMO) gaining prominence. While these newer technologies offer advanced support capabilities, IABP remains a valuable option due to its relative simplicity, ease of insertion, and minimal risk of complications. In comparison to other support devices, IABP is less invasive and can be inserted at the bedside, making it an attractive choice for initial stabilization of critically ill patients.
Future Trends Projection: Advancements in IABP Technology
As with all medical technologies, IABP therapy continues to evolve. Future advancements are likely to focus on improving the ease of use, reducing complications, and enhancing patient outcomes. Some potential areas of development include:
- Enhanced Materials and Designs: Improvements in balloon materials and designs could lead to better durability and reduced risk of vascular complications.
- Automated Systems: The integration of artificial intelligence and automated systems could improve the synchronization of balloon inflation and deflation with the cardiac cycle, potentially leading to better clinical outcomes.
- Minimally Invasive Techniques: Advancements in minimally invasive surgical techniques could further reduce the risk associated with IABP insertion.
Decision Framework: Initiating IABP Therapy
The decision to initiate IABP therapy should be made cautiously, considering the patient’s clinical status, the likelihood of benefiting from the therapy, and the potential risks. A systematic approach involves:
- Assessment of the Patient’s Condition: Evaluating the severity of cardiac dysfunction and the potential for recovery.
- Review of Clinical Guidelines: Adhering to established guidelines and recommendations for IABP use.
- Multidisciplinary Consultation: Consulting with cardiologists, cardiothoracic surgeons, and other relevant specialists to determine the best course of action.
- Informed Consent: Ensuring that the patient or their surrogate is fully informed about the procedure, its benefits, and its risks.
Resource Guide: Management of IABP Therapy
Effective management of IABP therapy requires a comprehensive approach that includes:
- Monitoring: Continuous monitoring of the patient’s hemodynamic status, including blood pressure, cardiac output, and signs of organ perfusion.
- Adjustments: Regular adjustments of the IABP settings to optimize support and minimize potential complications.
- Complication Management: Prompt recognition and management of complications, such as balloon rupture, vascular injury, or thrombocytopenia.
- Weaning: A gradual weaning process once the patient’s condition stabilizes, to assess the heart’s ability to function independently.
FAQ Section
What are the primary indications for IABP therapy?
+The primary indications include cardiogenic shock, acute myocardial infarction complicated by shock or severe ischemia, and mechanical complications of AMI, among others.
How does IABP therapy support the heart?
+IABP therapy supports the heart by inflating a balloon in the aorta during diastole, which increases aortic pressure and enhances coronary perfusion, and deflating it during systole, reducing afterload and facilitating the heart's pumping action.
What are the potential complications of IABP therapy?
+Potential complications include vascular injury, thrombocytopenia, balloon rupture, and infection. Prompt recognition and management of these complications are crucial for optimizing patient outcomes.
Can IABP therapy be used in conjunction with other mechanical support devices?
+Yes, IABP therapy can be used in conjunction with other mechanical support devices, such as ECMO or VADs, depending on the patient's clinical needs and the judgment of the healthcare team.
What is the process for weaning a patient off IABP therapy?
+The process for weaning a patient off IABP therapy involves gradually reducing the level of support provided by the IABP while closely monitoring the patient's hemodynamic status. This is typically done once the patient's condition has stabilized and there is evidence of improved cardiac function.
Conclusion
IABP therapy represents a vital component in the management of severe cardiac conditions, offering a bridge to recovery or further intervention for patients in critical need. As medical technology continues to evolve, the role of IABP therapy will likely undergo changes, with advancements aimed at improving efficacy, reducing complications, and enhancing patient outcomes. Through a comprehensive understanding of its principles, indications, and management, healthcare providers can optimize the use of IABP therapy, ultimately contributing to better care for patients with complex cardiac diseases.