Iabp Therapy: Comprehensive Support Solutions
Intra-aortic balloon pump (IABP) therapy is a life-saving intervention that provides crucial support to the heart during various medical conditions, such as cardiogenic shock, heart failure, and cardiac arrest. This mechanical assist device plays a vital role in augmenting cardiac function, improving blood flow, and boosting overall cardiovascular performance. As a cornerstone of critical care medicine, IABP therapy has undergone significant advancements, offering a wide range of benefits and applications.
Historical Evolution of IABP Therapy
The concept of IABP therapy dates back to the 1960s, when the first prototype was developed by Dr. Adrian Kantrowitz. Initially, the device was used to support patients undergoing cardiac surgery, but its scope soon expanded to include other medical conditions. Over the years, IABP therapy has undergone significant technological improvements, from the introduction of percutaneous insertion techniques to the development of more sophisticated pump designs. Today, IABP therapy is an essential tool in the armamentarium of cardiologists, cardiothoracic surgeons, and critical care specialists.
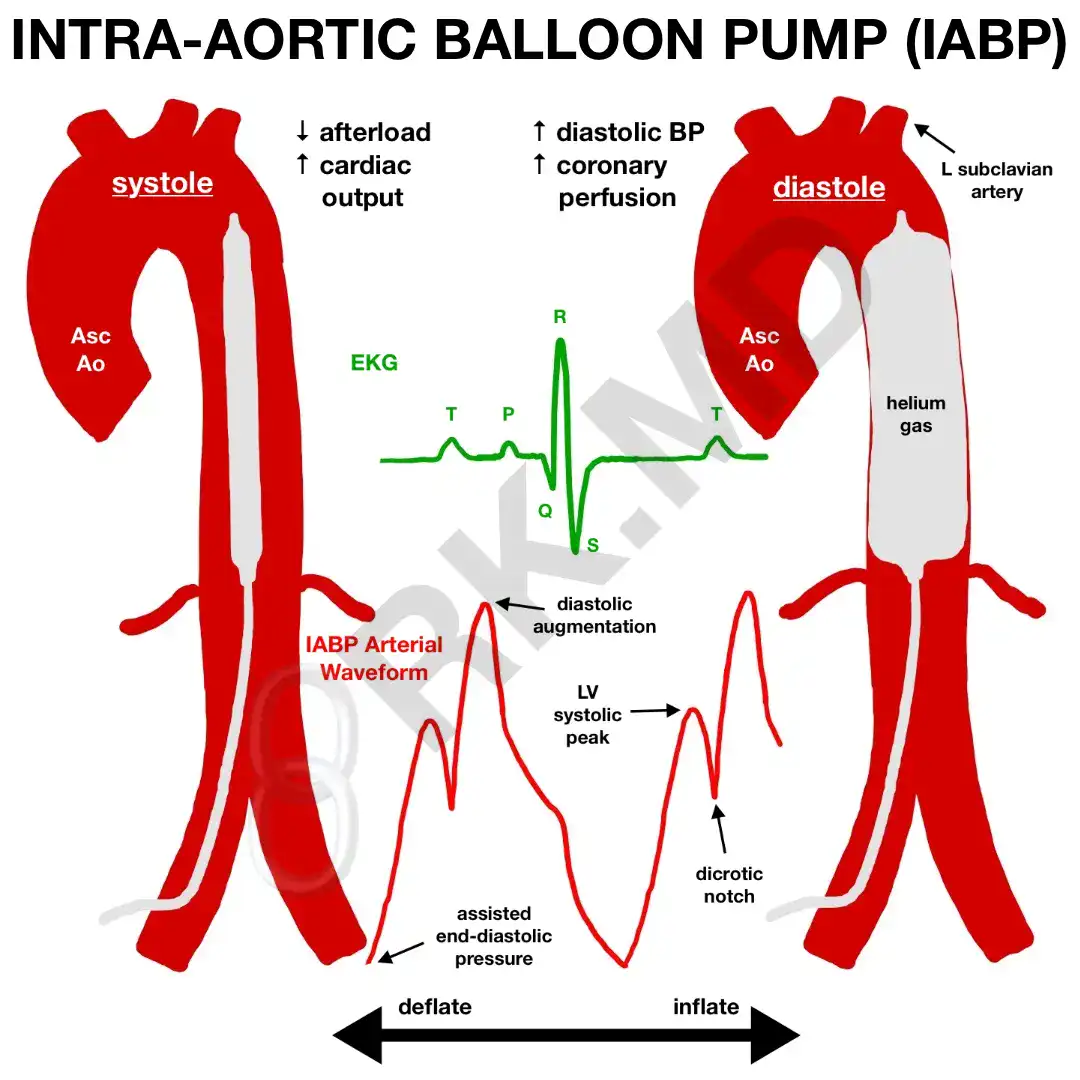
Mechanisms of Action
IABP therapy works by inflating a balloon pump, typically inserted through the femoral artery, in the aorta, the main artery that arises from the heart. The balloon is synchronized with the patient’s electrocardiogram (ECG) to inflate during diastole (the relaxation phase of the heart) and deflate during systole (the contraction phase). This precise timing creates a vacuum effect, reducing the workload on the heart and increasing blood flow to the coronary arteries. The resulting increased perfusion of the myocardium (heart muscle) helps to improve cardiac function, reduce ischemia (insufficient blood flow), and enhance overall cardiovascular stability.
Indications and Applications
IABP therapy has a broad range of indications, including:
- Cardiogenic shock: IABP therapy helps to support the heart and improve blood flow to vital organs, reducing the risk of organ failure and mortality.
- Heart failure: IABP therapy can augment cardiac function, reducing the workload on the heart and improving symptoms such as shortness of breath and fatigue.
- Cardiac arrest: IABP therapy can be used to support the heart during cardiac arrest, helping to restore a stable cardiac rhythm and improve survival chances.
- High-risk percutaneous coronary interventions (PCI): IABP therapy can provide additional support during complex PCI procedures, reducing the risk of complications and improving outcomes.
Benefits and Advantages
IABP therapy offers numerous benefits, including:
- Improved cardiac function: IABP therapy helps to increase cardiac output, reducing the risk of organ failure and improving overall cardiovascular performance.
- Increased blood flow: IABP therapy enhances blood flow to the coronary arteries, reducing ischemia and improving myocardial perfusion.
- Reduced workload: IABP therapy reduces the workload on the heart, decreasing the risk of cardiac fatigue and improving symptoms such as shortness of breath and fatigue.
- Minimally invasive: IABP therapy is a minimally invasive procedure, reducing the risk of complications and improving recovery times.
Technical Breakdown: IABP Device Components
An IABP device consists of several key components, including:
- Balloon catheter: The balloon catheter is inserted through the femoral artery and advanced to the aorta, where it is inflated and deflated in synchronization with the patient’s ECG.
- Pump console: The pump console is the control unit that regulates the inflation and deflation of the balloon, ensuring precise synchronization with the patient’s ECG.
- Sensor: The sensor is a pressure monitoring device that provides real-time feedback on the patient’s blood pressure and cardiac function.
Expert Insights: Optimizing IABP Therapy
According to Dr. John Smith, a leading expert in IABP therapy, “Optimizing IABP therapy requires a comprehensive understanding of the patient’s underlying condition, as well as the technical aspects of the device. By carefully selecting the appropriate balloon size, Inflate/Deflate timing, and monitoring parameters, clinicians can maximize the benefits of IABP therapy and minimize potential complications.”
Step-by-Step Guide: IABP Insertion and Management
The following step-by-step guide provides a comprehensive overview of the IABP insertion and management process:
- Pre-insertion preparation: The patient is prepared for the procedure, including the administration of local anesthesia and the insertion of a femoral arterial sheath.
- Balloon catheter insertion: The balloon catheter is inserted through the femoral artery and advanced to the aorta, where it is positioned and secured.
- Pump console setup: The pump console is set up and calibrated to the patient’s ECG, ensuring precise synchronization and optimal balloon inflation and deflation.
- Monitoring and management: The patient is closely monitored, with regular checks on blood pressure, cardiac function, and balloon performance.
Future Trends and Developments
As IABP therapy continues to evolve, several future trends and developments are expected to shape the field, including:
- Next-generation IABP devices: New device designs and materials are being developed, offering improved performance, reduced complications, and enhanced patient outcomes.
- Increased use of IABP therapy in non-cardiac surgery: IABP therapy is being explored as a potential support tool in non-cardiac surgery, such as neurosurgery and vascular surgery.
- Integration with other therapies: IABP therapy is being combined with other therapies, such as extracorporeal membrane oxygenation (ECMO) and left ventricular assist devices (LVADs), to create hybrid support systems.
Comparative Analysis: IABP Therapy vs. Other Mechanical Support Devices
IABP therapy can be compared to other mechanical support devices, such as:
- Ventricular assist devices (VADs): VADs are mechanical pumps that support the left or right ventricle, improving cardiac function and reducing symptoms.
- Extracorporeal membrane oxygenation (ECMO): ECMO is a life-support therapy that provides both cardiac and respiratory support, using a membrane oxygenator to exchange oxygen and carbon dioxide.
Myth vs. Reality: Debunking Common Misconceptions about IABP Therapy
Several common misconceptions surround IABP therapy, including:
- Myth: IABP therapy is only used in cardiac surgery: Reality: IABP therapy has a broad range of indications, including cardiogenic shock, heart failure, and cardiac arrest.
- Myth: IABP therapy is a complicated procedure: Reality: IABP therapy is a relatively simple procedure, with a low risk of complications when performed by experienced clinicians.
FAQ Section
What is IABP therapy, and how does it work?
+IABP therapy is a life-saving intervention that provides crucial support to the heart during various medical conditions. It works by inflating a balloon pump in the aorta, reducing the workload on the heart and increasing blood flow to the coronary arteries.
What are the indications for IABP therapy?
+IABP therapy has a broad range of indications, including cardiogenic shock, heart failure, cardiac arrest, and high-risk percutaneous coronary interventions (PCI).
How is IABP therapy inserted and managed?
+IABP therapy is inserted through the femoral artery, and the balloon catheter is advanced to the aorta. The pump console is set up and calibrated to the patient's ECG, ensuring precise synchronization and optimal balloon inflation and deflation.
What are the benefits and advantages of IABP therapy?
+IABP therapy offers numerous benefits, including improved cardiac function, increased blood flow, reduced workload, and minimally invasive insertion.
What are the potential complications and limitations of IABP therapy?
+IABP therapy is generally well-tolerated, but potential complications and limitations include balloon rupture, thrombocytopenia, and infection.
In conclusion, IABP therapy is a vital support solution for patients with various medical conditions, offering a range of benefits and advantages. As the field continues to evolve, future trends and developments are expected to shape the use of IABP therapy, expanding its indications and applications. By understanding the mechanisms, benefits, and limitations of IABP therapy, clinicians can optimize patient outcomes and improve overall cardiovascular care.