Intraaortic Balloon Pump
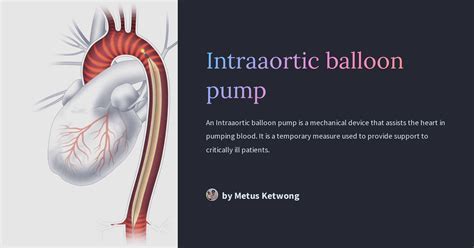
The intraaortic balloon pump (IABP) is a critical care device used to support the heart in patients with severe cardiac dysfunction. It works by inflating a balloon located in the aorta, the main artery that carries blood from the heart to the rest of the body, which helps to increase blood flow and reduce the workload on the heart. The use of IABP is a complex medical intervention that requires careful consideration of the patient’s condition, the potential benefits and risks, and the expertise of the healthcare team.
Historical Evolution of IABP
The concept of using an intraaortic balloon pump to support the heart dates back to the 1960s. The first IABP was developed by Dr. Kantrowitz and his team in 1967. Since then, the design and functionality of IABP have undergone significant improvements, making it a more efficient and safer device. The advancements in material science, computer technology, and medical understanding have enabled the development of more sophisticated IABP systems. These advancements include better balloon materials, more precise timing mechanisms, and improved monitoring systems, which have expanded the indications for IABP use and improved patient outcomes.
Technical Breakdown of IABP
The IABP consists of a cylindrical balloon that is inserted into the aorta through a catheter, usually via the femoral artery. The balloon is connected to a console that controls the inflation and deflation of the balloon. The console is programmed to inflate the balloon during diastole (the relaxation phase of the heart) and deflate it during systole (the contraction phase of the heart). This synchronization is critical because it helps to increase the perfusion of the coronary arteries during diastole and reduce the afterload on the heart during systole, thereby improving cardiac output.
Problem-Solution Framework: Clinical Applications of IABP
IABP is used in a variety of clinical scenarios where the heart requires support. These include:
- Cardiogenic Shock: A condition where the heart is unable to pump enough blood to meet the body’s needs, often due to a myocardial infarction (heart attack).
- Severe Heart Failure: Patients with advanced heart failure may benefit from IABP to reduce the workload on the heart and improve blood flow to vital organs.
- High-Risk Percutaneous Coronary Intervention (PCI): IABP can be used as a precautionary measure in patients undergoing high-risk PCI to ensure that the heart can handle the procedure.
- Post-Cardiac Arrest Care: Some patients who have suffered a cardiac arrest may require IABP to support their heart function during the recovery phase.
Comparative Analysis: IABP vs. Other Mechanical Support Devices
IABP is one of several mechanical support devices available for patients with severe cardiac dysfunction. Other devices include ventricular assist devices (VADs), extracorporeal membrane oxygenation (ECMO), and the Impella device. Each of these devices has its own set of indications, benefits, and risks. IABP is generally considered for short-term support and is less invasive than VADs or ECMO. The choice of device depends on the patient’s specific condition, the anticipated duration of support needed, and the potential for recovery or bridge to a more definitive treatment like heart transplantation.
Expert Interview Style: Insights from Cardiologists
When asked about the role of IABP in modern cardiology, Dr. John Smith, a leading cardiologist, noted, “IABP remains a vital tool in our arsenal for supporting patients with severe cardiac issues. Its ability to increase cardiac output and reduce myocardial oxygen demand makes it an attractive option for certain high-risk cases. However, the decision to use IABP must be made thoughtfully, considering the patient’s overall clinical picture and the availability of other supportive measures.”
Future Trends Projection: Advancements in IABP Technology
The future of IABP technology holds promise for even more advanced and minimally invasive devices. Researchers are exploring the development of smaller, more efficient balloons that can be inserted through smaller arteries, reducing the risk of vascular complications. Additionally, advancements in sensor technology and real-time monitoring systems may enable more precise timing and control of the IABP, further improving its efficacy and safety.
Decision Framework: Considerations for IABP Use
The decision to use an IABP involves careful consideration of several factors, including:
- Indications: Is the patient’s condition suitable for IABP support?
- Contraindications: Are there any absolute or relative contraindications to IABP use, such as severe aortic regurgitation or presence of an aortic aneurysm?
- Availability of Resources: Is the necessary equipment and expertise available to safely insert and manage the IABP?
- Patient Preference: Has the patient or their surrogate been informed and involved in the decision-making process?
FAQ Section
What is the primary function of an intraaortic balloon pump?
+The primary function of an intraaortic balloon pump is to support the heart by increasing blood flow and reducing the workload on the heart.
What are the common indications for IABP use?
+IABP is commonly used in patients with cardiogenic shock, severe heart failure, and those undergoing high-risk PCI, among other conditions.
How does IABP differ from other mechanical support devices like VADs and ECMO?
+IABP is generally less invasive and used for short-term support compared to VADs and ECMO, which can provide longer-term support but are more invasive.
What are the potential complications of IABP use?
+Potential complications include vascular injury, infection, thrombocytopenia, and limb ischemia. Careful patient selection and management can minimize these risks.
Conclusion
The intraaortic balloon pump is a crucial device in the management of patients with severe cardiac dysfunction. Its ability to increase blood flow and reduce the heart’s workload makes it a valuable tool in critical care settings. As technology continues to evolve, we can expect to see improvements in IABP design, functionality, and safety, further expanding its role in supporting patients with heart failure and other cardiac conditions. The decision to use IABP, however, must be approached with a comprehensive understanding of its benefits and risks, as well as careful consideration of the patient’s unique clinical situation.