Intraaortic Balloon Pump Guide: Expert Insights
The intraaortic balloon pump (IABP) has been a cornerstone of cardiac care for decades, providing critical support to patients with severe cardiac disease. This complex medical device is designed to increase myocardial oxygen perfusion and decrease cardiac afterload, making it an indispensable tool in the management of various cardiac conditions. However, the effective use of an IABP requires a deep understanding of its principles, applications, and potential complications.
Historical Evolution of Intraaortic Balloon Pumps
The concept of the IABP was first introduced in the 1960s, with the first clinical use reported in 1968. Since its inception, the IABP has undergone significant technological advancements, transforming from a bulky, console-based system to a more compact, user-friendly device. These advancements have not only improved the safety and efficacy of IABP therapy but have also expanded its applications in clinical practice. Today, IABPs are used in a wide range of settings, from coronary care units to operating rooms, for conditions such as acute myocardial infarction, cardiogenic shock, and during high-risk coronary interventions.
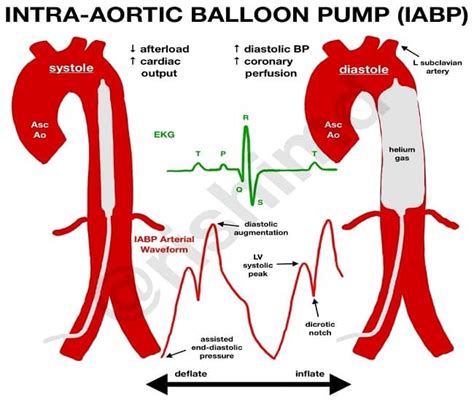
How Intraaortic Balloon Pumps Work
The IABP operates on the principle of counterpulsation, where a balloon is inserted into the aorta and inflated during diastole, increasing blood pressure in the aorta and thereby enhancing coronary artery perfusion. Simultaneously, the balloon deflates during systole, reducing afterload and facilitating left ventricular ejection. This dual action improves the myocardial oxygen supply-demand balance, which is critical for maintaining cardiac function in compromised patients. The timing of balloon inflation and deflation is synchronized with the patient’s cardiac cycle, typically using the electrocardiogram (ECG) or arterial pressure waveform as a trigger.
Indications and Contraindications for IABP Use
The decision to use an IABP is based on a comprehensive assessment of the patient’s clinical condition, including the severity of cardiac dysfunction, the presence of contraindications, and the potential benefits and risks of therapy. Common indications for IABP support include acute myocardial infarction with cardiogenic shock, refractory angina, and high-risk coronary interventions. On the other hand, contraindications may include severe aortic regurgitation, aortic dissection, and peripheral arterial disease that could preclude safe insertion of the balloon catheter.
Technical Breakdown: Insertion and Management of IABPs
The insertion of an IABP typically involves percutaneous placement of a balloon catheter via the femoral artery, guided by fluoroscopy. Once in place, the balloon is inflated with helium or carbon dioxide, and its operation is monitored using a console that controls the timing and pressure of inflation and deflation. Proper management of the IABP requires continuous monitoring of the patient’s hemodynamic status, including arterial pressure, cardiac output, and indices of myocardial oxygenation. Adjustments to the balloon pump settings may be necessary to optimize cardiac support while minimizing the risk of complications.
Complications and Limitations of IABP Therapy
While the IABP is a valuable therapeutic tool, its use is not without risks. Potential complications include vascular injury at the site of insertion, limb ischemia, bleeding, and infection. Moreover, the IABP may not be effective in all patients, particularly those with severe cardiac dysfunction or contraindications to its use. Therefore, careful patient selection, meticulous technique during insertion, and vigilant monitoring during therapy are essential to minimize risks and maximize benefits.
Future Trends and Innovations in IABP Technology
As medical technology continues to evolve, we can expect significant advancements in IABP design and functionality. Future developments may include more compact and user-friendly devices, improved materials for balloon construction, and advanced sensors for real-time monitoring of cardiac function. Additionally, there may be a greater emphasis on developing IABP systems that can be used in a broader range of clinical settings, including community hospitals and even outpatient environments.
Decision Framework for IABP Use
The decision to use an IABP should be based on a structured approach that considers the patient’s clinical profile, the potential benefits of therapy, and the risks and limitations of the device. This framework should include:
- Clinical Assessment: Evaluate the severity of cardiac disease and the presence of indications for IABP support.
- Risk Stratification: Assess the patient’s risk profile, including the presence of contraindications and potential complications.
- Alternative Therapies: Consider alternative therapeutic options, such as pharmacological support or mechanical circulatory assistance with other devices.
- Multidisciplinary Consultation: Involve a team of healthcare professionals, including cardiologists, intensivists, and cardiothoracic surgeons, in the decision-making process.
Pro-Con Analysis of IABP Therapy
Pros:
- Enhanced Cardiac Support: IABPs provide critical support to the failing heart, improving myocardial oxygenation and reducing afterload.
- Versatility: IABPs can be used in a variety of clinical settings and for different cardiac conditions.
- Reversible: IABP support is reversible, allowing for the potential for cardiac recovery.
Cons:
- Invasive Procedure: Insertion of an IABP is an invasive procedure with associated risks.
- Complications: Potential complications, including vascular injury and infection, can be severe.
- Requires Expertise: Effective management of an IABP requires specialized knowledge and skills.
Step-by-Step Guide to IABP Insertion
- Prepare the Patient: Ensure the patient is appropriately prepared, including the administration of anticoagulation and analgesia as needed.
- Access the Femoral Artery: Obtain access to the femoral artery using a percutaneous approach under fluoroscopic guidance.
- Insert the Balloon Catheter: Advance the balloon catheter through the femoral artery and into the aorta.
- Position the Balloon: Position the balloon in the descending aorta, approximately 2 cm below the origin of the left subclavian artery.
- Initiate IABP Therapy: Initiate IABP therapy, synchronizing the balloon inflation and deflation with the patient’s cardiac cycle.
FAQ Section
What are the primary indications for intraaortic balloon pump support?
+The primary indications for intraaortic balloon pump (IABP) support include acute myocardial infarction with cardiogenic shock, refractory angina, and high-risk coronary interventions.
How does an intraaortic balloon pump work?
+An intraaortic balloon pump (IABP) works by inflating a balloon in the aorta during diastole, which increases blood pressure in the aorta and enhances coronary artery perfusion. The balloon deflates during systole, reducing afterload and facilitating left ventricular ejection.
What are the potential complications of intraaortic balloon pump therapy?
+Potential complications of intraaortic balloon pump (IABP) therapy include vascular injury at the site of insertion, limb ischemia, bleeding, and infection. Proper management and monitoring are crucial to minimize these risks.
In conclusion, the intraaortic balloon pump remains a vital tool in the arsenal of cardiac care, offering critical support to patients with severe cardiac disease. As technology continues to evolve, we can expect to see advancements in IABP design, functionality, and clinical applications. By understanding the principles, indications, and management of IABP therapy, healthcare professionals can optimize its use, minimizing risks and maximizing benefits for patients in need.



