Losing Weight Pre Diabetes: Eat To Prevent Full Diabetes
Pre-diabetes is a condition where blood sugar levels are higher than normal, but not high enough to be classified as diabetes. This condition can often be managed and even reversed through lifestyle changes, including dietary adjustments. One of the primary goals for individuals with pre-diabetes is to prevent the progression to full blown diabetes, and weight loss can play a crucial role in this endeavor.
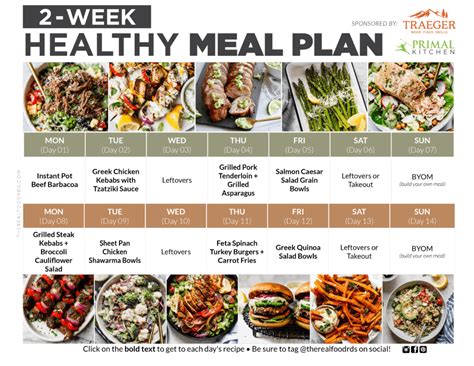
For those looking to lose weight and prevent diabetes, the key is to focus on sustainable, long-term lifestyle changes rather than quick fixes or fad diets. This involves adopting a balanced eating plan that is rich in whole, unprocessed foods such as vegetables, fruits, whole grains, lean proteins, and healthy fats. These foods provide essential nutrients, fiber, and satiety, which can help regulate blood sugar levels and support weight loss.
One effective approach is to follow a Mediterranean-style diet, which has been shown to have numerous health benefits, including weight management and improved insulin sensitivity. This dietary pattern emphasizes whole grains, fruits, vegetables, lean proteins, and healthy fats, such as those found in olive oil. It also encourages moderate consumption of dairy products and red wine, and limits intake of red meat and processed foods.
In addition to the types of foods consumed, portion control and meal frequency can also play a significant role in weight loss and diabetes prevention. Eating smaller, more frequent meals throughout the day can help regulate blood sugar levels and prevent excessive hunger, which can lead to overeating. It’s also important to pay attention to serving sizes and control the amount of food consumed at each meal.
Regular physical activity is also crucial for weight loss and diabetes prevention. Aim for at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, per week. Additionally, incorporate strength-training exercises, high-intensity interval training (HIIT), and other forms of physical activity to help improve insulin sensitivity and overall health.
It’s also important to stay hydrated by drinking plenty of water throughout the day. Sometimes, thirst can be mistaken for hunger, leading to unnecessary snacking and calorie consumption. Drinking water before meals can also help with portion control and reduce the likelihood of overeating.
For individuals with pre-diabetes, monitoring carbohydrate intake is also essential. Choosing complex, fiber-rich carbohydrates such as whole grains, fruits, and vegetables, and limiting refined and processed carbohydrates, can help regulate blood sugar levels. The glycemic index (GI) is a useful tool for determining the impact of different foods on blood sugar levels. Foods with a low GI, such as oats, barley, and most fruits and vegetables, are digested and absorbed slowly, causing a gradual increase in blood sugar levels.
Foods with a high GI, such as white bread, sugary snacks, and sweetened beverages, are digested and absorbed quickly, causing a rapid spike in blood sugar levels. It’s best to limit or avoid these foods altogether.
Expert Tip: Keeping track of carbohydrate intake and monitoring blood sugar levels can be a helpful way to manage pre-diabetes and prevent the progression to full-blown diabetes. Consult with a healthcare provider or registered dietitian to develop a personalized meal plan that takes into account individual nutritional needs and health goals.
Another crucial aspect of diabetes prevention is getting enough sleep. Poor sleep quality and duration have been linked to an increased risk of developing insulin resistance and type 2 diabetes. Aim for 7-9 hours of sleep per night and prioritize good sleep hygiene, such as avoiding caffeine and electronics before bedtime, and creating a relaxing sleep environment.
Stress management is also essential for overall health and diabetes prevention. Chronic stress can raise cortisol levels, which can contribute to insulin resistance and weight gain. Engage in stress-reducing activities, such as yoga, meditation, or deep breathing exercises, to help manage stress and promote relaxation.
Step-by-Step Guide to Managing Pre-Diabetes through Diet and Lifestyle:
- Focus on whole, unprocessed foods, including vegetables, fruits, whole grains, lean proteins, and healthy fats.
- Choose complex, fiber-rich carbohydrates and limit refined and processed carbohydrates.
- Monitor carbohydrate intake and keep track of blood sugar levels.
- Aim for regular physical activity, including aerobic exercise, strength training, and high-intensity interval training (HIIT).
- Stay hydrated by drinking plenty of water throughout the day.
- Prioritize good sleep hygiene and aim for 7-9 hours of sleep per night.
- Engage in stress-reducing activities, such as yoga, meditation, or deep breathing exercises.
In conclusion, losing weight and preventing diabetes requires a multifaceted approach that incorporates dietary changes, regular physical activity, stress management, and adequate sleep. By focusing on whole, unprocessed foods, monitoring carbohydrate intake, and engaging in regular physical activity, individuals with pre-diabetes can reduce their risk of developing full-blown diabetes and improve their overall health and well-being.
What is the best diet for pre-diabetes?
+A Mediterranean-style diet that emphasizes whole grains, fruits, vegetables, lean proteins, and healthy fats is a good starting point. It’s essential to focus on whole, unprocessed foods and limit refined and processed carbohydrates.
Can I reverse pre-diabetes through diet and lifestyle changes?
+Yes, it is possible to reverse pre-diabetes through diet and lifestyle changes. By losing weight, increasing physical activity, and improving insulin sensitivity, individuals can reduce their risk of developing full-blown diabetes.
How can I monitor my blood sugar levels and track my progress?
+Consult with a healthcare provider or registered dietitian to develop a personalized plan for monitoring blood sugar levels and tracking progress. This may include regular blood glucose monitoring, tracking food intake and physical activity, and regular check-ins with a healthcare provider.