Lyme Disease Blood Test Results Decoded
Understanding the intricacies of Lyme disease blood test results can be a daunting task, even for medical professionals. The complexity arises from the various types of tests available, each measuring different aspects of the immune system’s response to the bacteria that cause Lyme disease, Borrelia burgdorferi. This article aims to demystify the process of interpreting these test results, providing a comprehensive guide for both patients and healthcare providers.
Introduction to Lyme Disease Testing
Lyme disease is a multi-systemic infection caused by the spirochete Borrelia burgdorferi, which is transmitted to humans through the bite of infected black-legged ticks (Ixodes scapularis). The disease manifests in stages, starting with an early localized phase, often marked by a distinctive skin rash known as erythema migrans, followed by an early disseminated phase, and potentially progressing to a late disseminated phase if left untreated. The diagnosis of Lyme disease is primarily clinical, relying on the presence of symptoms and history of exposure. However, laboratory tests play a critical role in confirming the diagnosis, especially during the later stages of the disease when the rash may have resolved.
Types of Lyme Disease Tests
There are several types of tests used to diagnose Lyme disease, each with its own set of indications, advantages, and limitations. The most common tests include:
Enzyme-Linked Immunosorbent Assay (ELISA): This is the most frequently used initial test for Lyme disease. It measures the levels of antibodies (IgM and IgG) against B. burgdorferi in the blood. IgM antibodies typically appear early in the disease, while IgG antibodies are seen later and can persist for months after successful treatment.
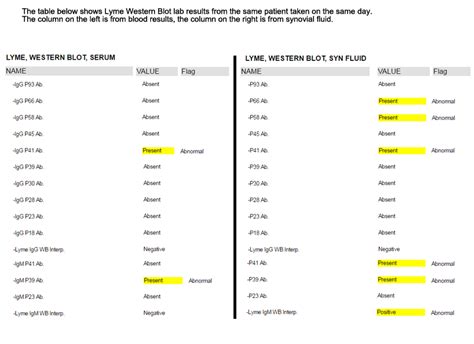
Western Blot: This test is often used to confirm the diagnosis when the ELISA test is positive or equivocal. Western blot can distinguish between IgM and IgG antibodies and can identify the specific proteins (bands) that these antibodies are directed against. The presence of certain bands is considered diagnostic for Lyme disease.
Polymerase Chain Reaction (PCR): This test detects the genetic material (DNA) of B. burgdorferi directly. It is primarily used for patients with Lyme arthritis or meningitis, as these conditions are associated with the presence of the bacteria in the joint or cerebrospinal fluid.
Decoding Test Results
Interpreting Lyme disease blood test results requires understanding the significance of the different antibodies and their timing in relation to the disease’s progression.
IgM Positive, IgG Negative: This pattern is typically seen in the early stages of the disease, usually within the first few weeks after infection. A positive IgM result can indicate recent exposure to B. burgdorferi.
IgM Negative, IgG Positive: This pattern is associated with later stages of the disease or past infection. The presence of IgG antibodies indicates that the immune system has had time to mount a more sustained response, which can occur weeks to months after the initial infection.
Both IgM and IgG Positive: This can be seen in patients with early disseminated or late-stage Lyme disease, reflecting an ongoing immune response to the infection.
Understanding False Negatives and False Positives
False negatives can occur early in the disease before the body has produced enough antibodies to be detected or in patients who have been taking antibiotics, which can suppress the immune response. False positives can result from cross-reactivity with other bacteria or from the presence of antibodies from a past, successfully treated infection.
The Role of Clinical Judgment
Laboratory tests should always be interpreted in the context of clinical symptoms and history of tick exposure. A healthcare provider may diagnose Lyme disease based on clinical presentation even if the test results are negative, especially during the early stages when antibody levels may not have risen sufficiently to be detected.
Strategies for Accurate Diagnosis
- Clinical Evaluation: A thorough medical history and physical examination are crucial for suspecting Lyme disease.
- Test Selection: Choosing the right test at the right time based on the stage of the disease and the patient’s symptoms.
- Interpretation of Results: Understanding the limitations and potential false results of each test.
- Repeat Testing: May be necessary if the initial test is negative but clinical suspicion remains high.
Conclusion
Decoding Lyme disease blood test results is a nuanced process that requires a deep understanding of the disease’s progression, the immune system’s response, and the limitations of diagnostic tests. By combining clinical acumen with a thorough grasp of laboratory testing, healthcare providers can make accurate diagnoses and provide timely, effective treatment for patients with Lyme disease.
FAQ Section
What is the most common test for diagnosing Lyme disease?
+The Enzyme-Linked Immunosorbent Assay (ELISA) is the most frequently used initial test for diagnosing Lyme disease, measuring the levels of antibodies against B. burgdorferi in the blood.
How long after a tick bite can Lyme disease be detected by a blood test?
+It can take a few weeks after the tick bite for antibodies against B. burgdorferi to develop and be detectable by blood tests. Early treatment based on clinical symptoms may be initiated before test results are available.