Newborn Blood Sugar: Expert Monitoring Guide
The arrival of a newborn is a life-changing event, and as new parents, it’s natural to feel concerned about the health and well-being of your baby. One essential aspect of newborn care is monitoring blood sugar levels, as low blood sugar (hypoglycemia) can be a serious condition that requires prompt attention. In this comprehensive guide, we’ll delve into the world of newborn blood sugar monitoring, exploring the importance of blood sugar control, the risks associated with hypoglycemia, and the best practices for monitoring and managing blood sugar levels in newborns.
Understanding Newborn Blood Sugar
Newborns, especially those who are premature or have certain medical conditions, are at risk of developing hypoglycemia due to their immature glucose regulation systems. After birth, babies rely on their stored glycogen and glucose from their mother’s milk or formula to maintain their blood sugar levels. However, if the newborn’s glucose demands exceed their glucose supply, their blood sugar levels can drop, leading to hypoglycemia.
The Risks of Hypoglycemia in Newborns
Hypoglycemia can have serious consequences for newborns, including:
- Brain damage: Prolonged or severe hypoglycemia can cause brain damage, leading to developmental delays, learning disabilities, or even seizures.
- Organ damage: Hypoglycemia can also damage other organs, such as the heart, liver, or kidneys.
- Increased risk of infection: Newborns with hypoglycemia are more susceptible to infections, which can further exacerbate their condition.
Monitoring Blood Sugar Levels in Newborns
To prevent or detect hypoglycemia, healthcare providers use various methods to monitor blood sugar levels in newborns. These methods include:
- Blood glucose meters: These devices measure the concentration of glucose in a blood sample.
- Continuous glucose monitoring systems: These systems involve inserting a small sensor under the skin to track glucose levels continuously.
- Heel pricks: A quick and minimally invasive method to collect a blood sample from the heel of the newborn.
When to Monitor Blood Sugar Levels
The frequency and timing of blood sugar monitoring depend on various factors, including:
- Age: Newborns under 24 hours old require more frequent monitoring.
- Feeding schedule: Monitor blood sugar levels before and after feedings to ensure adequate glucose intake.
- Medical conditions: Newborns with certain medical conditions, such as hypothyroidism or heart defects, may require more frequent monitoring.
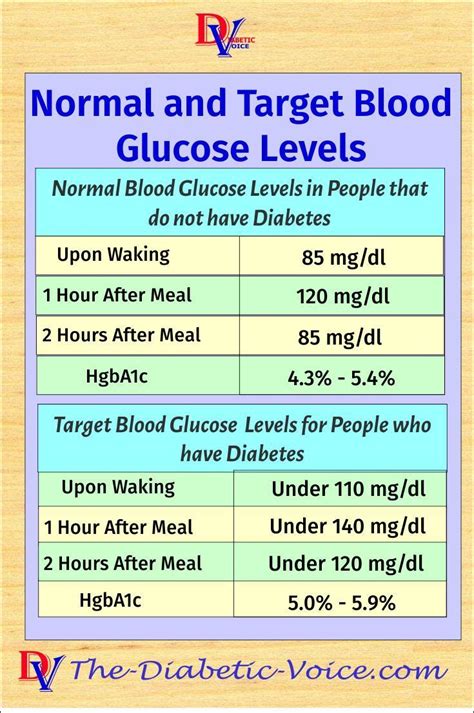
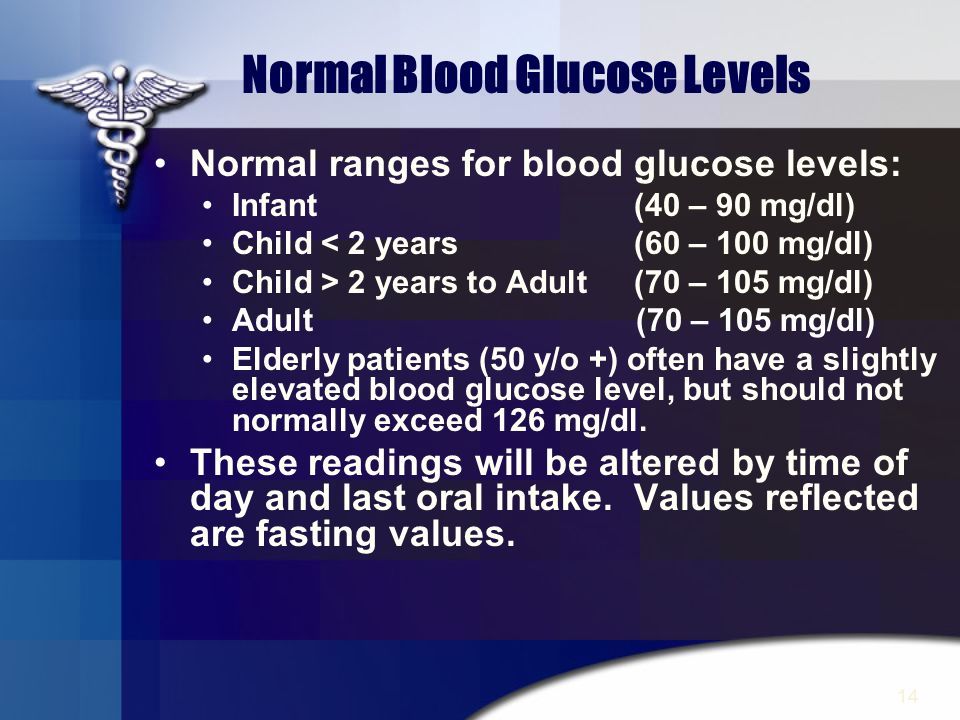
Interpreting Blood Sugar Results
When interpreting blood sugar results, healthcare providers consider the following ranges:
- Normal: 54-145 mg/dL (3.0-8.0 mmol/L)
- Mild hypoglycemia: 40-53 mg/dL (2.2-2.9 mmol/L)
- Moderate hypoglycemia: 30-39 mg/dL (1.6-2.1 mmol/L)
- Severe hypoglycemia: <30 mg/dL (<1.6 mmol/L)
Managing Hypoglycemia in Newborns
If a newborn is diagnosed with hypoglycemia, treatment typically involves:
- Oral glucose gel: A quick-acting glucose gel administered orally to raise blood sugar levels.
- Intravenous glucose: For more severe cases, glucose is administered through an IV line.
- Frequent feedings: Increasing the frequency and volume of feedings to ensure adequate glucose intake.
It's essential for new parents to work closely with their healthcare provider to monitor and manage their newborn's blood sugar levels. By being aware of the risks and taking proactive steps, you can help ensure your baby's health and well-being.
Prevention Strategies
While monitoring and treatment are crucial, preventing hypoglycemia is also important. Strategies include:
- Breastfeeding: Breast milk provides optimal glucose and nutrient intake for newborns.
- Frequency and volume of feedings: Ensuring adequate feedings to meet the newborn’s glucose demands.
- Monitoring for risk factors: Identifying and addressing potential risk factors, such as prematurity or certain medical conditions.
Pros and Cons of Continuous Glucose Monitoring Systems
| Pros | Cons |
|---|---|
| Provides continuous glucose data | May cause skin irritation or allergic reactions |
| Enables timely interventions | Requires frequent sensor replacements |
| Improves glucose control and reduces hypoglycemia risk | May be costly and not covered by insurance |
Frequently Asked Questions
What are the symptoms of hypoglycemia in newborns?
+Symptoms of hypoglycemia in newborns may include lethargy, jitteriness, seizures, poor feeding, and pale or blue-tinged skin.
How often should I monitor my newborn's blood sugar levels?
+The frequency of monitoring depends on your newborn's age, feeding schedule, and medical conditions. Consult with your healthcare provider to determine the best monitoring schedule for your baby.
Can I prevent hypoglycemia in my newborn?
+While not all cases of hypoglycemia can be prevented, breastfeeding, frequent feedings, and monitoring for risk factors can help reduce the risk of hypoglycemia in newborns.
As a new parent, it’s essential to be aware of the importance of monitoring blood sugar levels in your newborn. By understanding the risks and taking proactive steps, you can help ensure your baby’s health and well-being. Remember to work closely with your healthcare provider to develop a personalized monitoring and management plan tailored to your newborn’s unique needs. With the right guidance and support, you can navigate the challenges of newborn care and provide the best possible start for your baby.