Nissen Fundoplication Surgery
The Nissen fundoplication, a type of surgical procedure, has been a cornerstone in the treatment of gastroesophageal reflux disease (GERD) for decades. This surgery, named after Dr. Rudolf Nissen, who first described the technique in the 1950s, is designed to strengthen the barrier between the esophagus and the stomach, preventing the reflux of stomach acid into the esophagus. The procedure involves wrapping the upper portion of the stomach (fundus) around the lower portion of the esophagus to create a valve-like mechanism that prevents acid reflux.
Historical Evolution of the Nissen Fundoplication
The concept of surgically treating GERD has undergone significant evolution since the first Nissen fundoplication was performed. Initially, the procedure was quite invasive, requiring a large incision in the abdomen. However, with advancements in medical technology and surgical techniques, the procedure has become less invasive. The introduction of laparoscopic surgery in the 1990s marked a significant turning point, allowing for smaller incisions and quicker recovery times. Today, the Nissen fundoplication can be performed using minimally invasive techniques, including robotic-assisted surgery, which offers improved precision and reduced risk of complications.
Technical Breakdown of the Procedure
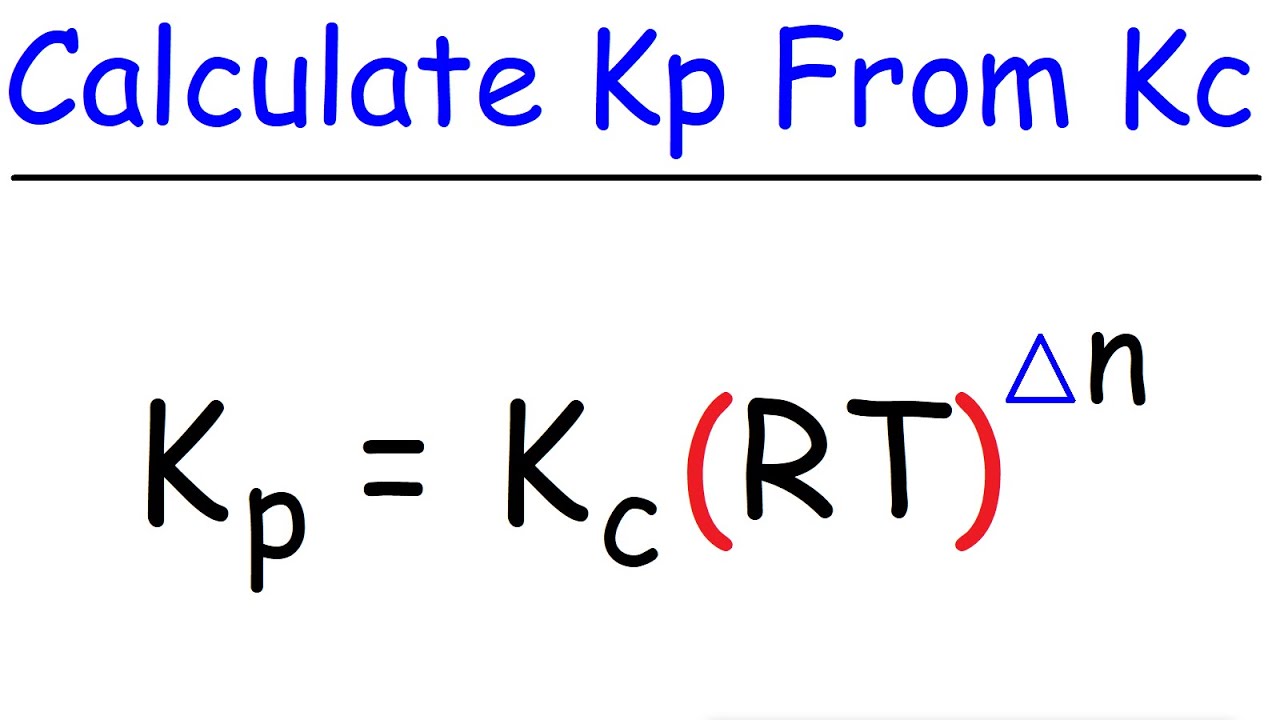
The Nissen fundoplication procedure, whether performed openly or laparoscopically, involves several key steps. First, the patient is placed under general anesthesia to ensure comfort during the surgery. The surgeon then makes several small incisions in the abdomen through which a laparoscope (a thin, lighted tube with a camera) and surgical instruments are inserted. The stomach is then mobilized, and the fundus is wrapped 360 degrees around the lower esophagus. The wrap is typically secured with sutures, and sometimes, a bougie (a thin, flexible tube) is used to help size the wrap correctly. The goal is to create a tight enough wrap to prevent reflux but not so tight that it causes difficulty swallowing.
One of the critical aspects of the Nissen fundoplication is the proper sizing of the wrap. If the wrap is too loose, it may not effectively prevent acid reflux, while a wrap that is too tight can lead to dysphagia (difficulty swallowing). Achieving the right balance is key to the success of the procedure.
Problem-Solution Framework: Addressing Complications and Limitations
While the Nissen fundoplication is an effective treatment for GERD, it is not without potential complications and limitations. Common issues include dysphagia, gas-bloat syndrome (inability to belch), and wrap migration or slippage. To address these challenges, surgeons have developed several strategies, including the use of partial wraps (such as the Toupet fundoplication) for patients at risk of dysphagia and the implementation of rigorous post-operative care plans to manage symptoms and prevent long-term complications.
Post-Operative Care and Recovery
- Immediate Recovery: Patients typically spend one to three days in the hospital after surgery, during which time they are closely monitored for complications.
- Dietary Changes: A gradual transition from a liquid diet to soft foods and eventually to a normal diet is recommended to minimize discomfort and prevent straining the wrap.
- Follow-Up Appointments: Regular follow-up with the surgeon is crucial to assess the effectiveness of the procedure and address any emerging issues.
Comparative Analysis: Nissen Fundoplication vs. Other Treatment Options
The treatment landscape for GERD is diverse, ranging from lifestyle modifications and medical therapy to various surgical interventions. The Nissen fundoplication is often compared to other surgical options, such as the LINX Reflux Management System, which involves implanting a ring of magnetic beads to reinforce the lower esophageal sphincter, and to medical management with proton pump inhibitors (PPIs). Each approach has its benefits and drawbacks. The Nissen fundoplication is generally considered for patients who have severe symptoms, significant esophageal damage, or those who have not responded well to medical therapy. However, it is a more invasive procedure compared to the LINX system and carries a higher risk of complications.
What are the primary indications for a Nissen fundoplication?
+The primary indications include severe gastroesophageal reflux disease (GERD) that is refractory to medical therapy, significant esophageal complications such as strictures or Barrett's esophagus, and for some patients, symptoms that significantly impact quality of life despite optimal medical management.
How effective is the Nissen fundoplication in treating GERD?
+The Nissen fundoplication is highly effective in treating GERD, with success rates ranging from 80% to 90% in eliminating symptoms and healing esophageal inflammation. However, long-term results can vary, and some patients may experience recurrence of symptoms over time.
Future Trends Projection: Evolving Surgical Techniques and Technologies
The field of surgical treatment for GERD is continually evolving, with advancements in technology and techniques offering new possibilities for patients. Robotic surgery, for example, is becoming more prevalent, allowing for enhanced precision and potentially better outcomes. Additionally, there is ongoing research into less invasive procedures and new materials that could further improve the effectiveness and durability of anti-reflux surgeries. The future of GERD treatment may also involve a more personalized approach, with genetic and physiological factors guiding the selection of the most appropriate treatment strategy for each individual.
Conclusion:
The Nissen fundoplication has established itself as a reliable and effective surgical treatment for GERD, offering a significant improvement in quality of life for many patients. As with any medical procedure, it is not without risks and complications, and the decision to undergo surgery should be made in consultation with a healthcare provider, considering all treatment options and individual circumstances. As medical science continues to advance, it is likely that the techniques and technologies surrounding the Nissen fundoplication will evolve, potentially leading to even better outcomes for patients suffering from this common and debilitating condition.