As we delve into the intricacies of blood glucose management, it’s essential to understand the dynamics at play. For individuals with diabetes, maintaining healthy blood glucose levels is a delicate balancing act that requires a deep understanding of the physiological processes involved. The body’s ability to regulate blood sugar levels is a complex interplay of hormonal signals, metabolic pathways, and lifestyle factors.
At the heart of this regulation is the hormone insulin, produced by the pancreas, which plays a crucial role in glucose uptake and storage. In individuals with diabetes, this insulin-regulated process is disrupted, leading to elevated blood glucose levels. The consequences of unmanaged diabetes can be severe, ranging from cardiovascular disease and nerve damage to kidney failure and blindness. Therefore, it’s critical for diabetics to monitor and manage their blood glucose levels meticulously.
Understanding Blood Glucose Levels
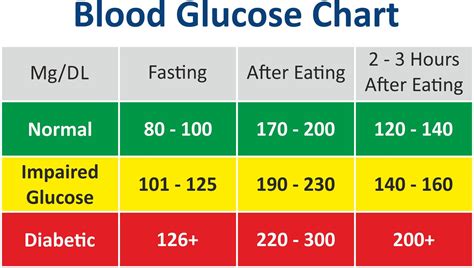
Blood glucose levels are measured in milligrams per deciliter (mg/dL) and are categorized into several ranges:
- Normal Fasting Blood Glucose: Below 100 mg/dL. This range indicates that the body is efficiently managing blood sugar levels, even after an overnight fast.
- Impaired Fasting Glucose: Between 100 mg/dL and 125 mg/dL. Individuals within this range are at an increased risk of developing type 2 diabetes and cardiovascular disease.
- Diabetes: 126 mg/dL or higher. This level confirms the presence of diabetes, highlighting the need for lifestyle adjustments and possibly medication to manage the condition.
For individuals with diabetes, the American Diabetes Association recommends the following target blood glucose levels:
- Before meals: 80-130 mg/dL
- After meals (1-2 hours): Less than 180 mg/dL
Achieving these targets requires a multifaceted approach, including dietary management, regular physical activity, and, if prescribed, medication.
Dietary Management
A well-planned diet is the cornerstone of diabetes management. It involves balancing carbohydrate intake with protein and healthy fats to maintain stable blood glucose levels. Key dietary considerations include:
- Carbohydrate counting: Tracking the amount of carbohydrates consumed to predict their impact on blood glucose levels.
- Glycemic Index (GI): Choosing foods with a low GI, which cause a slower and smaller rise in blood glucose levels.
- Meal frequency and timing: Eating regular, balanced meals to maintain stable energy levels and prevent spikes in blood glucose.
Physical Activity
Regular physical activity is another critical component of diabetes management. Exercise improves insulin sensitivity, allowing glucose to enter cells more efficiently. This can lead to better blood glucose control and a reduced risk of complications. The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic exercise, or 75 minutes of vigorous-intensity aerobic exercise, or a combination of both, per week.
Monitoring and Medication
Regular monitoring of blood glucose levels is essential for understanding how different factors, such as diet and exercise, affect glucose levels. This information can be used to make informed decisions about lifestyle adjustments and, if necessary, to adjust medication regimens.
For many individuals with diabetes, medication is a crucial aspect of their management plan. This can include metformin, sulfonylureas, meglitinides, thiazolidinediones, SGLT2 inhibitors, and GLP-1 receptor agonists, among others. Each medication works in a different way to help the body regulate blood glucose levels, and the choice of medication depends on the type of diabetes, the presence of other health conditions, and the individual’s lifestyle.
Lifestyle Adjustments
Beyond diet, exercise, and medication, several lifestyle adjustments can help manage diabetes:
- Stress management: High levels of stress can increase cortisol levels, leading to higher blood glucose. Practices like yoga, meditation, and deep breathing exercises can help manage stress.
- Sleep hygiene: Getting adequate sleep is crucial for glucose regulation. Most adults need 7-8 hours of sleep per night.
- Smoking cessation: Smoking can worsen diabetes complications. Quitting smoking can significantly improve health outcomes.
Conclusion
Managing diabetes is a lifelong commitment that requires dedication, patience, and a deep understanding of the factors that influence blood glucose levels. By combining dietary management, regular physical activity, monitoring, and, when necessary, medication, individuals with diabetes can achieve healthy blood glucose levels, reducing the risk of complications and improving their quality of life. It’s a journey that involves continuous learning, adaptation, and a proactive approach to health, but with the right strategies and support, it’s possible to thrive with diabetes.
What are the normal blood glucose levels for individuals without diabetes?
+Normal fasting blood glucose levels are below 100 mg/dL. After eating, levels should be less than 140 mg/dL. These levels indicate that the body is effectively regulating blood sugar.
How often should I check my blood glucose levels if I have diabetes?
+The frequency of checking blood glucose levels depends on the type of diabetes and the treatment plan. Generally, individuals with type 1 diabetes and some with type 2 diabetes may need to check their levels several times a day, while others may need to check less frequently. It’s essential to follow the advice of your healthcare provider.
What are the risks of high blood glucose levels for individuals with diabetes?
+High blood glucose levels over time can lead to serious complications, including heart disease, stroke, kidney disease, nerve damage, and blindness. Managing blood glucose levels is crucial to prevent these complications.
Can lifestyle changes alone manage diabetes, or is medication always necessary?
+Lifestyle changes, including diet and exercise, are fundamental in managing diabetes. For some individuals, especially those with type 2 diabetes, these changes can be enough to manage the condition. However, many people will also need medication to achieve their target blood glucose levels. The need for medication depends on the severity of the diabetes, the individual’s overall health, and how well lifestyle changes alone can manage blood glucose levels.
How can I prevent diabetes if I have a family history of the disease?
+If you have a family history of diabetes, you can reduce your risk by maintaining a healthy weight, engaging in regular physical activity, eating a balanced diet that is low in sugar and saturated fats, and avoiding smoking. Regular health check-ups can also help in early detection and management of prediabetes or diabetes.