Pancreatitis Explained: Comprehensive Guide Inside
Pancreatitis, a condition characterized by inflammation of the pancreas, is a complex and multifaceted disorder that affects thousands of people worldwide. The pancreas, an organ located behind the stomach, plays a crucial role in digestion and metabolism, producing enzymes that help break down food and hormones like insulin and glucagon that regulate blood sugar levels. When the pancreas becomes inflamed, it can lead to a range of symptoms, from mild discomfort to life-threatening complications. In this comprehensive guide, we will delve into the world of pancreatitis, exploring its causes, symptoms, diagnosis, treatment options, and management strategies.
Understanding the Pancreas and Pancreatitis
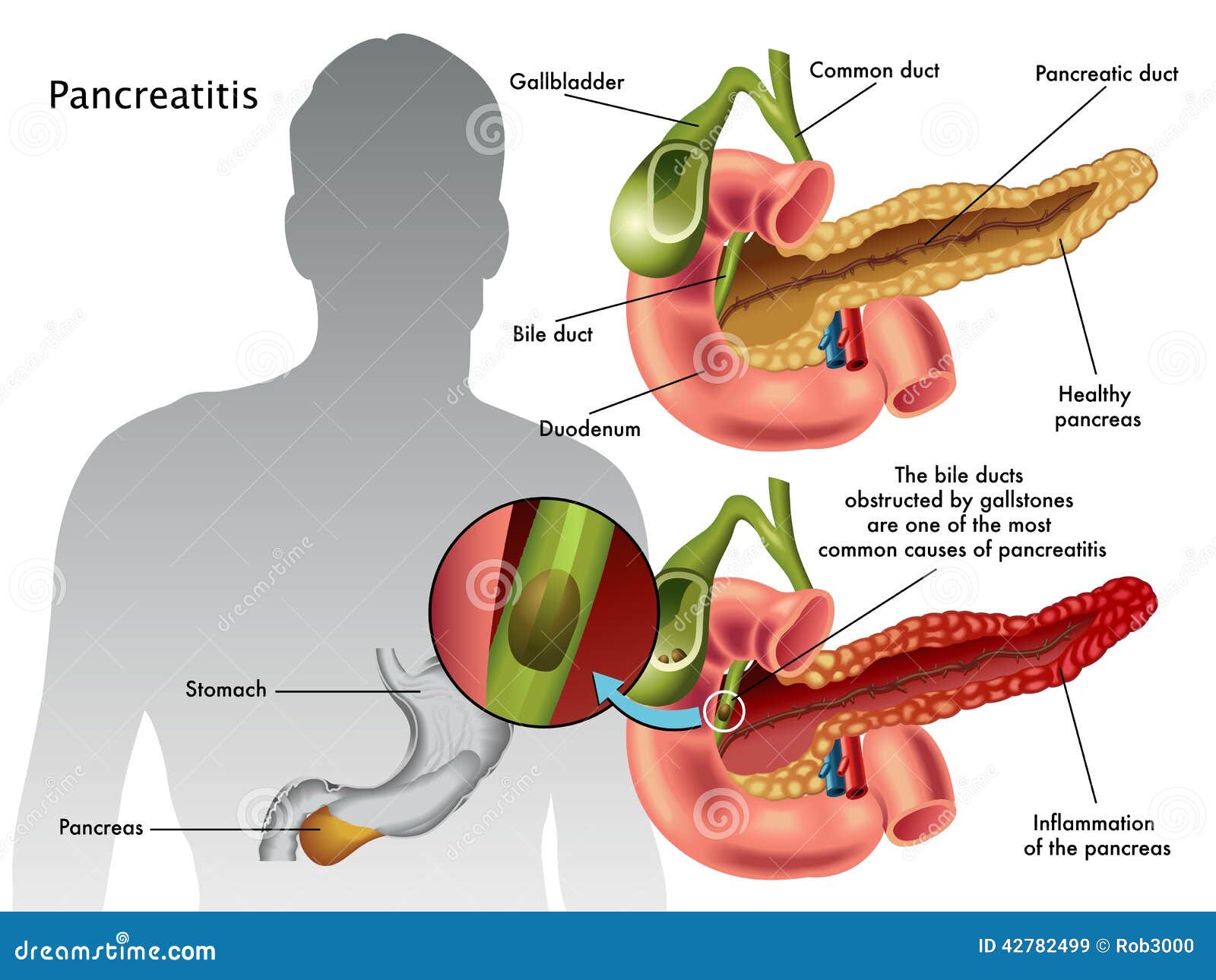
To grasp the concept of pancreatitis, it’s essential to understand the pancreas’s function and structure. The pancreas is composed of two main types of cells: exocrine cells, which produce digestive enzymes, and endocrine cells, which produce hormones. When the pancreas becomes inflamed, it can affect both exocrine and endocrine functions, leading to a range of symptoms.
There are two primary forms of pancreatitis: acute and chronic. Acute pancreatitis is a sudden inflammation of the pancreas, often caused by gallstones or excessive alcohol consumption. Chronic pancreatitis, on the other hand, is a long-term inflammation of the pancreas, which can lead to permanent damage and scarring.
Causes and Risk Factors
Pancreatitis can be caused by a variety of factors, including:
- Gallstones: Gallstones are a common cause of acute pancreatitis, as they can block the pancreatic duct and trigger inflammation.
- Alcohol consumption: Excessive alcohol consumption is a significant risk factor for chronic pancreatitis, as it can cause inflammation and scarring in the pancreas.
- Genetic disorders: Certain genetic disorders, such as cystic fibrosis, can increase the risk of developing pancreatitis.
- Infections: Viral or bacterial infections, such as mumps or malaria, can cause pancreatitis.
- Medications: Certain medications, such as corticosteroids and certain antibiotics, can increase the risk of developing pancreatitis.
- Trauma: Physical trauma to the abdomen, such as from a car accident, can cause pancreatitis.
Symptoms and Diagnosis
The symptoms of pancreatitis can vary depending on the type and severity of the condition. Common symptoms include:
- Abdominal pain: Severe, persistent pain in the upper abdomen is a hallmark symptom of pancreatitis.
- Nausea and vomiting: Many people with pancreatitis experience nausea and vomiting, which can lead to dehydration and electrolyte imbalances.
- Fever: A high fever can indicate an infection or inflammation in the pancreas.
- Swollen abdomen: The abdomen may become swollen and tender to the touch.
Diagnosing pancreatitis can be challenging, as the symptoms can be similar to those of other conditions. A combination of physical examination, medical history, and diagnostic tests, such as:
- Blood tests: Blood tests can measure the levels of pancreatic enzymes, such as amylase and lipase, which can indicate inflammation.
- Imaging tests: Imaging tests, such as CT scans or MRI, can help visualize the pancreas and detect any abnormalities.
- Endoscopic ultrasound: An endoscopic ultrasound can help diagnose pancreatitis and detect any blockages or damage to the pancreatic duct.
Treatment Options
Treatment for pancreatitis depends on the type and severity of the condition. For acute pancreatitis, treatment typically involves:
- Pain management: Medications, such as painkillers and anti-inflammatory drugs, can help manage pain and inflammation.
- Fluid replacement: Intravenous fluids can help replace lost fluids and electrolytes.
- Nutritional support: A balanced diet and nutritional supplements can help support the healing process.
- Antibiotics: If an infection is present, antibiotics may be prescribed to treat the underlying infection.
For chronic pancreatitis, treatment may involve:
- Pain management: Medications, such as painkillers and anti-inflammatory drugs, can help manage pain and inflammation.
- Enzyme replacement: Supplements can help replace lost pancreatic enzymes, improving digestion and nutrient absorption.
- Dietary changes: A balanced diet and lifestyle changes, such as avoiding alcohol and smoking, can help manage symptoms and slow disease progression.
- Surgery: In some cases, surgery may be necessary to remove damaged tissue or repair any blockages in the pancreatic duct.
Management Strategies
While there is no cure for pancreatitis, there are several management strategies that can help alleviate symptoms and slow disease progression. These include:
- Dietary changes: A balanced diet that is low in fat and high in fiber can help manage symptoms and improve digestion.
- Avoiding triggers: Avoiding triggers, such as alcohol and certain medications, can help prevent flare-ups.
- Stress management: Stress management techniques, such as meditation and deep breathing, can help reduce stress and anxiety.
- Regular exercise: Regular exercise, such as walking or yoga, can help improve overall health and well-being.
Conclusion
Pancreatitis is a complex and multifaceted condition that requires a comprehensive approach to management. By understanding the causes, symptoms, diagnosis, treatment options, and management strategies, individuals with pancreatitis can take control of their condition and improve their quality of life. Remember, pancreatitis is a serious condition that requires prompt medical attention. If you or someone you know is experiencing symptoms of pancreatitis, seek medical help immediately.
What are the symptoms of pancreatitis?
+The symptoms of pancreatitis can vary depending on the type and severity of the condition, but common symptoms include abdominal pain, nausea and vomiting, fever, and swollen abdomen.
How is pancreatitis diagnosed?
+Diagnosing pancreatitis can be challenging, but a combination of physical examination, medical history, and diagnostic tests, such as blood tests, imaging tests, and endoscopic ultrasound, can help diagnose the condition.
What are the treatment options for pancreatitis?
+Treatment for pancreatitis depends on the type and severity of the condition, but may involve pain management, fluid replacement, nutritional support, antibiotics, enzyme replacement, dietary changes, and surgery.
How can I manage pancreatitis?
+While there is no cure for pancreatitis, management strategies, such as dietary changes, avoiding triggers, stress management, and regular exercise, can help alleviate symptoms and slow disease progression.
Is pancreatitis a serious condition?
+Yes, pancreatitis is a serious condition that requires prompt medical attention. If left untreated, pancreatitis can lead to life-threatening complications, such as infection, bleeding, and organ failure.



