Pericardial Effusion Guide: Know The Signs
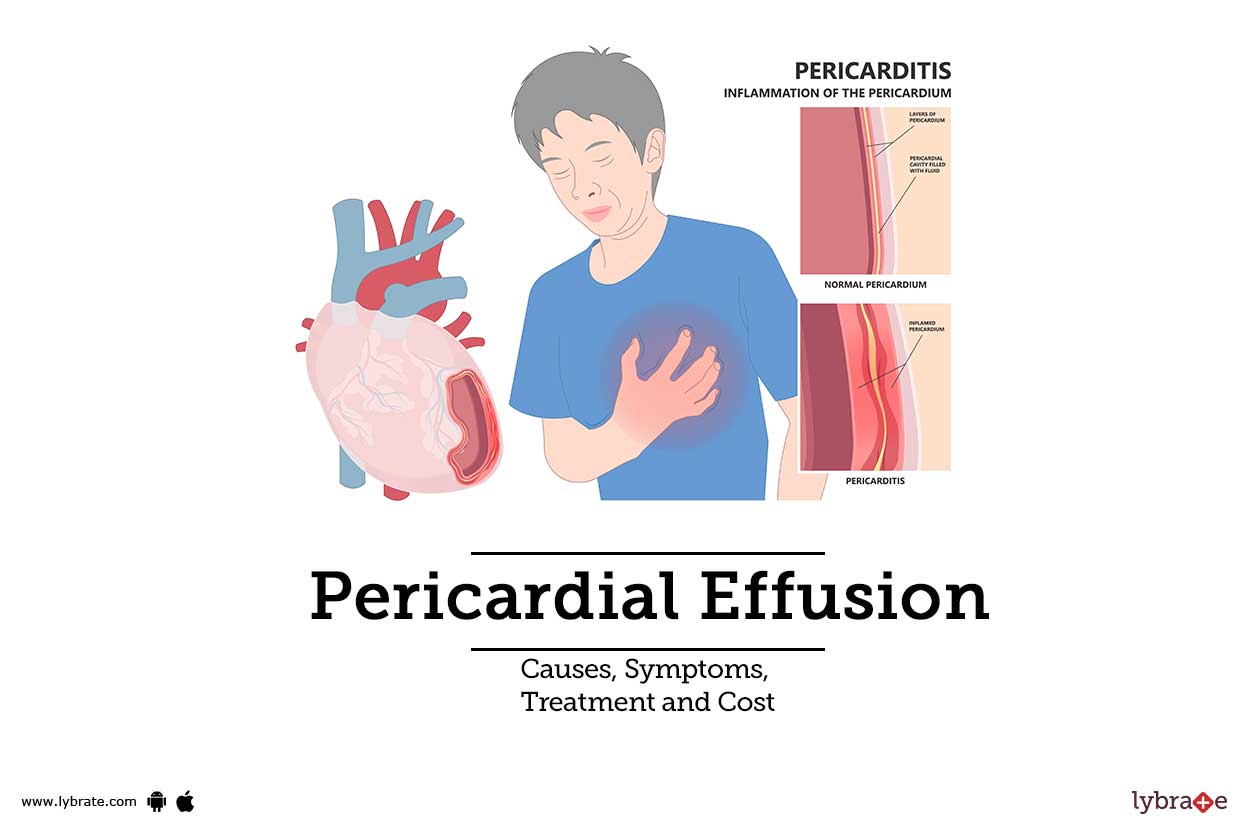
The pericardium, a fibroserous sac surrounding the heart, plays a vital role in maintaining cardiac function. However, when it becomes filled with an abnormal amount of fluid, a condition known as pericardial effusion occurs. This can be a life-threatening situation if left untreated, as the fluid accumulation can compress the heart, hindering its ability to pump blood effectively. Recognizing the signs and symptoms of pericardial effusion is crucial for timely medical intervention. In this comprehensive guide, we will delve into the world of pericardial effusion, exploring its causes, symptoms, diagnosis, treatment options, and management strategies.
Understanding Pericardial Effusion
Pericardial effusion is characterized by the accumulation of excess fluid within the pericardial space, which is the area between the pericardium and the heart. This fluid can be composed of various substances, including blood, pus, or serous fluid, depending on the underlying cause. The condition can be acute or chronic, with the acute form often presenting more dramatically due to the rapid accumulation of fluid. Chronic pericardial effusion, on the other hand, may develop gradually, sometimes without noticeable symptoms until the condition has significantly progressed.
Causes of Pericardial Effusion
The etiology of pericardial effusion is diverse, ranging from infectious diseases to malignancies and traumatic injuries. Some of the common causes include:
- Viral infections: Viral pericarditis can lead to the accumulation of fluid within the pericardial space.
- Bacterial infections: Bacterial pericarditis, often seen in the context of pneumonia or endocarditis, can cause pericardial effusion.
- Malignancies: Metastatic cancer to the pericardium or primary cardiac tumors can lead to effusion.
- Autoimmune disorders: Conditions such as lupus or rheumatoid arthritis can cause inflammation of the pericardium, leading to fluid accumulation.
- Trauma: Penetrating or blunt chest trauma can result in hemorrhage into the pericardial space.
Symptoms of Pericardial Effusion
The clinical presentation of pericardial effusion varies based on the volume and rate of fluid accumulation, as well as the underlying cause. Common symptoms include:
- Chest pain: This is often sharp and improves with sitting up and leaning forward.
- Shortness of breath: As the fluid compresses the heart, it can lead to decreased cardiac output, resulting in dyspnea.
- Fatigue: Reduced cardiac efficiency can cause generalized weakness.
- Palpitations: Patients may experience irregular heartbeats due to the heart’s compromised function.
- Cough: In some cases, especially with large effusions, patients may experience a dry cough due to the compression of airways or the lungs.
Diagnosis of Pericardial Effusion
Diagnosing pericardial effusion involves a combination of clinical assessment, imaging studies, and sometimes, invasive procedures. Key diagnostic tools include:
- Echocardiography: This is the primary imaging modality, allowing for the direct visualization of the pericardial fluid and assessment of its impact on cardiac function.
- Chest X-ray: May show an enlarged cardiac silhouette, known as a “water bottle” heart.
- Electrocardiogram (ECG): Can demonstrate low voltage QRS complexes or electrical alternans in the presence of a large effusion.
- Pericardiocentesis: Involves the aspiration of fluid from the pericardial space for diagnostic and therapeutic purposes.
Treatment and Management
The management of pericardial effusion depends on the underlying cause, the size of the effusion, and the presence of cardiac tamponade, a life-threatening condition where the heart is severely compressed. Treatment strategies may include:
- Pericardiocentesis: To drain the fluid and relieve tamponade.
- Pericardial window: A surgical procedure that creates a window in the pericardium to allow continuous drainage of fluid.
- Medical management: Addressing the underlying cause, such as treating infections or malignancies.
- Monitoring: Close observation of patients with small, asymptomatic effusions may be appropriate, especially if the cause is thought to be self-limiting.
Prognosis and Complications
The prognosis for pericardial effusion varies significantly depending on the underlying cause and the promptness and effectiveness of treatment. Untreated or inadequately managed pericardial effusion can lead to serious complications, including cardiac tamponade, which can be fatal. Recurrent effusions or the development of constrictive pericarditis are other potential complications.
Conclusion
Pericardial effusion is a complex condition that requires a thorough understanding of its causes, symptoms, and management strategies. Early recognition and intervention are critical to prevent serious complications and improve outcomes. By staying informed and vigilant, individuals can better navigate the challenges associated with pericardial effusion, ensuring timely medical attention when needed.
Frequently Asked Questions
What are the symptoms of pericardial effusion?
+The symptoms of pericardial effusion can include chest pain, shortness of breath, fatigue, palpitations, and cough. The severity of these symptoms can vary based on the size of the effusion and the underlying cause.
How is pericardial effusion diagnosed?
+Diagnosis of pericardial effusion involves clinical assessment, imaging studies such as echocardiography and chest X-ray, and sometimes, pericardiocentesis to directly visualize and sample the pericardial fluid.
What are the treatment options for pericardial effusion?
+Treatment options for pericardial effusion include pericardiocentesis to drain the fluid, medical management of the underlying cause, and in some cases, surgical intervention such as creating a pericardial window. The choice of treatment depends on the cause, size of the effusion, and the presence of complications like cardiac tamponade.
By understanding pericardial effusion, its clinical manifestations, diagnostic approaches, and therapeutic strategies, individuals can better appreciate the complexities of cardiac health and the importance of seeking medical care when symptoms arise. Remember, timely intervention is key to managing this condition effectively and preventing serious complications.