Period Pain Management Guide
The experience of period pain is a common aspect of life for many individuals who menstruate. It’s estimated that up to 80% of women and people who menstruate will face some level of discomfort during their menstrual cycle, with symptoms ranging from mild to severe. Despite its prevalence, period pain is often misunderstood and undertreated, leading to significant discomfort and disruption in daily life for those affected.
At the core of period pain management is a comprehensive understanding of its causes and the various mechanisms through which it can be addressed. Period pain, or dysmenorrhea, is primarily caused by the contraction of the uterus, which compresses nearby blood vessels and cuts off oxygen supply to the uterine tissue. This process triggers the release of pain-causing chemicals, known as prostaglandins, which stimulate the nerve endings in the uterus, leading to the sensation of pain. Additionally, hormonal changes during the menstrual cycle can also influence pain perception and contribute to the overall discomfort experienced.
Understanding Period Pain Types
Period pain is not a one-size-fits-all condition. It can vary significantly in intensity, duration, and nature, often categorized into two main types: primary and secondary dysmenorrhea.
Primary Dysmenorrhea: This is the most common form of period pain and typically begins 1-2 years after the onset of menstruation. It is characterized by cramping in the lower abdomen, often accompanied by other symptoms such as lower back pain, nausea, vomiting, diarrhea, and headache. Primary dysmenorrhea is caused by the production of prostaglandins and is usually treated with over-the-counter pain relievers and self-care practices.
Secondary Dysmenorrhea: This type of period pain develops later in life and is caused by an underlying medical condition, such as endometriosis, uterine fibroids, or pelvic inflammatory disease. The pain can be more severe and is often accompanied by heavy menstrual bleeding. Management of secondary dysmenorrhea requires treating the underlying condition and may involve more complex medical interventions.
Step-by-Step Management of Period Pain
Understand Your Body: Keeping a menstrual diary can help in identifying patterns and anticipating when period pain is likely to occur. This proactive approach allows for the implementation of preventive measures.
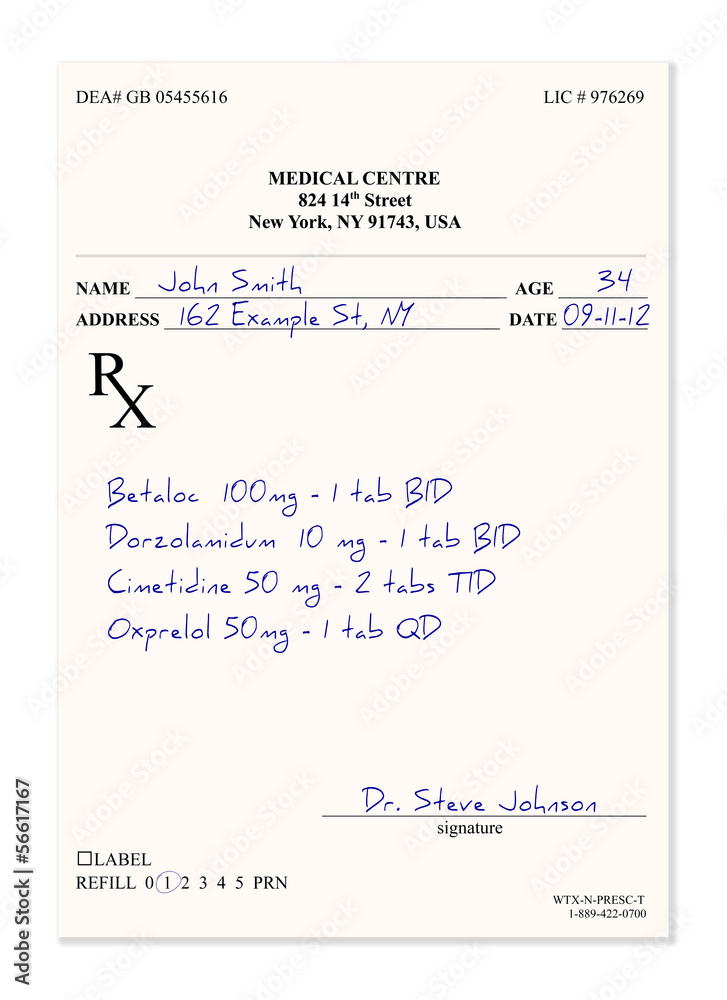
Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen are effective in reducing period pain by inhibiting the production of prostaglandins. They work best when taken as soon as symptoms appear or even before the onset of menstruation.
Heat Therapy: Applying heat to the lower abdomen can help relax the uterine muscles and improve blood flow, thus reducing pain. This can be achieved with a heating pad or a warm bath.
Exercise: Regular physical activity can reduce the severity of period pain. Activities such as yoga and swimming not only provide distraction but also release endorphins, which are the body’s natural painkillers.
Dietary Changes: Maintaining a balanced diet rich in fruits, vegetables, and whole grains can help in managing period pain. Foods rich in omega-3 fatty acids, such as fish, and those high in calcium, like dairy products, can also be beneficial.
Stress Management: High levels of stress can exacerbate period pain. Practices such as meditation, deep breathing, and progressive muscle relaxation can help reduce stress and alleviate discomfort.
Advanced Treatment Options
For individuals who experience severe period pain that does not respond to conventional treatments, several advanced management strategies are available:
Hormonal Treatments: Birth control pills, patches, and vaginal rings can help reduce or eliminate period pain by suppressing ovulation and reducing prostaglandin production.
Transcutaneous Electrical Nerve Stimulation (TENS): This involves the use of a small device that sends mild electrical pulses to the body via electrodes placed on the skin. TENS can help interrupt pain signals to the brain.
Acupuncture: This ancient practice involves the insertion of thin needles into specific points on the body to stimulate healing and pain relief. Acupuncture has been shown to be effective in managing period pain for some individuals.
Comparative Analysis of Treatment Options
When considering the various treatment options for period pain, it’s essential to evaluate their effectiveness, potential side effects, and suitability for individual circumstances. A comparative analysis reveals that while over-the-counter pain relievers are a common first line of defense, they may not be as effective for everyone, especially those with underlying conditions causing secondary dysmenorrhea. Hormonal treatments, on the other hand, can offer significant relief but may come with their own set of side effects and are not suitable for all individuals. Alternative therapies like acupuncture and heat therapy provide a more natural approach with minimal side effects but may vary in effectiveness from person to person.
Future Trends in Period Pain Management
The landscape of period pain management is evolving, with ongoing research exploring new and innovative approaches to alleviate discomfort and improve quality of life for those affected. Emerging trends include the development of non-invasive diagnostic tools to better understand the causes of period pain, the creation of personalized treatment plans based on genetic profiles and health data, and the integration of digital health technologies to monitor symptoms and provide real-time support.
Expert Insights: Moving Beyond Symptoms to Solutions
Expert authorities in the field of women’s health emphasize the importance of shifting the focus from merely managing symptoms to addressing the root causes of period pain. This involves not only educating individuals about their bodies and the options available for pain relief but also advocating for greater awareness and support within communities and healthcare systems.
“The experience of period pain is highly individualized, and what works for one person may not work for another. It’s crucial that we prioritize personalized care and empower individuals with the knowledge and resources they need to take control of their health.”
Decision Framework for Period Pain Management
When navigating the options for managing period pain, it’s helpful to have a structured approach to decision-making. This involves considering several key factors:
Severity of Pain: The intensity of the pain and its impact on daily life should guide the choice of treatment. Mild pain may be managed with self-care practices, while severe pain may require medical intervention.
Underlying Conditions: The presence of any underlying medical conditions should be taken into account. Conditions like endometriosis or uterine fibroids may require specific treatments.
Lifestyle Preferences: Personal preferences regarding hormonal treatments, surgical options, and alternative therapies should be considered.
Potential Side Effects: The potential side effects of any treatment should be weighed against its benefits.
Long-term Goals: Decisions should also consider long-term health goals, such as future fertility plans.
Key Takeaways
- Period pain is a common condition that affects a significant portion of the population who menstruate, varying in intensity and impact.
- Comprehensive management involves understanding the causes, adopting self-care practices, and when necessary, seeking medical treatment.
- A personalized approach, considering the individual’s health profile, lifestyle, and preferences, is crucial for effective pain management.
- Emerging trends and technologies offer promising solutions for the future, emphasizing the importance of ongoing research and awareness.
FAQ Section
What are the most effective over-the-counter medications for period pain?
+Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen are among the most effective over-the-counter medications for managing period pain. They work by reducing the production of prostaglandins, which are hormone-like substances that cause the uterus to contract and lead to pain.
How does exercise help in reducing period pain?
+Exercise can help reduce period pain through several mechanisms. It releases endorphins, which are the body's natural painkillers, and can help relax the uterine muscles, reducing cramping. Regular physical activity also improves overall health and reduces stress, which can contribute to the perception of pain.
What are some common myths about period pain?
+One common myth is that period pain is just a normal part of life and that individuals should tolerate it. Another myth is that hormonal treatments are always associated with significant side effects and should be avoided. It's essential to consult healthcare professionals to understand the facts and make informed decisions about health.
How can dietary changes impact period pain?
+Dietary changes can significantly impact period pain. Foods rich in omega-3 fatty acids, such as salmon, and those high in calcium, like dairy products and leafy greens, can help reduce inflammation and alleviate cramps. Avoiding triggers like caffeine and sugar, which can exacerbate symptoms, is also beneficial.
Are there any natural remedies for period pain that really work?
+Yes, several natural remedies have been shown to be effective in managing period pain. These include heat therapy, acupuncture, and certain herbal supplements like ginger and turmeric, which have anti-inflammatory properties. However, it's crucial to consult with a healthcare provider before adding any new supplements to your regimen.
In conclusion, period pain management is a multifaceted issue that requires a tailored approach, taking into account the individual’s unique health profile, lifestyle, and preferences. By combining self-care practices, medical treatments, and emerging technologies, individuals can find effective relief and improve their quality of life. As research continues to uncover the complexities of period pain, it’s essential to foster a supportive environment that encourages open dialogue, education, and innovation in healthcare.