Pneumothorax Chest Tube Management
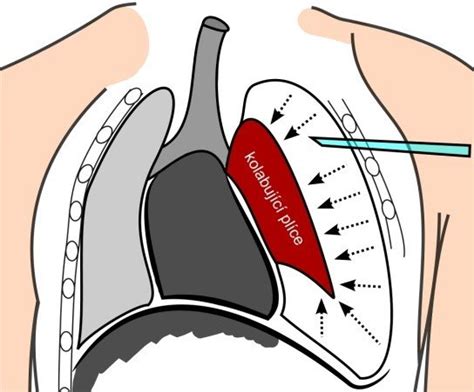
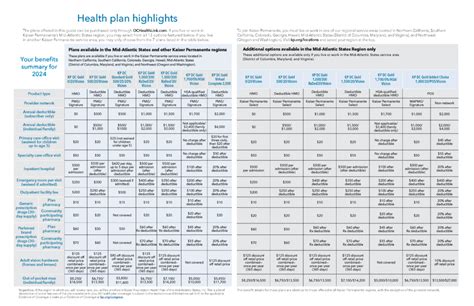
Pneumothorax, a condition characterized by the accumulation of air or gas in the pleural cavity, can lead to a collapse of the lung and is considered a medical emergency. The management of pneumothorax often involves the insertion of a chest tube, also known as a thoracostomy tube, to remove air and fluid from the pleural space, thereby allowing the lung to re-expand. Effective chest tube management is crucial for the treatment of pneumothorax and involves several key steps and considerations.
Understanding Pneumothorax
Before diving into the management of chest tubes in pneumothorax, it’s essential to understand the basics of the condition. Pneumothorax can be categorized into different types based on its cause and severity. These include spontaneous pneumothorax (which can be primary or secondary, depending on the presence of underlying lung disease), traumatic pneumothorax resulting from injury, and iatrogenic pneumothorax, which occurs as a complication of medical procedures. The choice of treatment, including the decision to insert a chest tube, depends on the type and severity of the pneumothorax, as well as the patient’s clinical condition.
Indications for Chest Tube Insertion
Chest tube insertion is indicated in several scenarios: - Large pneumothorax: When the pneumothorax is significant, and there’s a substantial collapse of the lung. - Tension pneumothorax: A life-threatening condition where air accumulates under pressure in the pleural space, pushing the mediastinum to the opposite side and compromising cardiorespiratory function. - Persistent air leak: In cases where there is an ongoing air leak from the lung into the pleural space. - Severe symptoms: Patients experiencing severe dyspnea, chest pain, or hemodynamic instability due to pneumothorax may require chest tube insertion.
Procedure for Insertion
The insertion of a chest tube is typically performed under local anesthesia. The procedure involves making an incision in the skin and muscles of the chest wall to access the pleural space. The tube is then inserted, and its position is confirmed with a chest X-ray. The choice of chest tube size depends on the patient’s size and the nature of the condition being treated. The tube is connected to an underwater seal drainage system, which allows air and fluid to escape from the pleural space while preventing air from entering.
Management of the Chest Tube
Monitoring and Care
- Drainage System: The underwater seal drainage system should be checked regularly to ensure that it is functioning correctly and that there is no air leak.
- Tube Security: The chest tube should be securely fastened to the skin with sutures or tape to prevent accidental dislodgement.
- Pain Management: Patients with chest tubes may experience significant pain and discomfort, requiring adequate analgesia.
- Infection Control: The insertion site should be monitored for signs of infection, and the chest tube should be handled aseptically.
Complications
Complications of chest tube insertion include: - Bleeding: Either from the site of tube insertion or from the lung parenchyma itself. - Infection: Pneumonia, empyema (infection of the pleural fluid), or wound infection at the site of tube insertion. - Injury to Surrounding Structures: Including the lung, major blood vessels, or nerves.
Removal of the Chest Tube
The decision to remove a chest tube is based on several factors, including: - Resolution of the Pneumothorax: Confirmed by chest X-ray showing full lung expansion and no significant residual air leak. - Clinical Stability: The patient should be clinically stable with no signs of respiratory distress. - Output: If the chest tube is placed for drainage of fluid, removal may be considered when the output decreases to a minimal amount over a 24-hour period.
Clinical Pearls
- Antibiotic Prophylaxis: Consideration should be given to the use of antibiotic prophylaxis at the time of chest tube insertion to reduce the risk of infection, although practices may vary.
- Follow-Up: Regular follow-up with chest X-rays is crucial to monitor the lung’s re-expansion and to detect any complications early.
- Patient Education: Patients should be educated on the signs of complications, such as increased pain, shortness of breath, or fever, and advised to seek medical attention immediately if they occur.
Conclusion
The management of pneumothorax with chest tubes is a critical aspect of thoracic care, requiring meticulous attention to detail and a comprehensive understanding of both the condition and the treatment modalities. By adhering to established protocols and being mindful of potential complications, healthcare providers can optimize patient outcomes and ensure the best possible results for those undergoing this treatment.
FAQ Section
What are the primary indications for chest tube insertion in pneumothorax?
+The primary indications include large pneumothorax, tension pneumothorax, persistent air leak, and severe symptoms such as dyspnea or chest pain.
How is the chest tube managed after insertion?
+Management involves monitoring the underwater seal drainage system, securing the tube to prevent dislodgement, managing pain, and watching for signs of infection.
What are the common complications of chest tube insertion?
+Common complications include bleeding, infection, and injury to surrounding structures such as the lung or major blood vessels.
When can a chest tube be removed?
+Removal is considered when the pneumothorax has resolved, the patient is clinically stable, and there is no significant air leak or fluid output.
By understanding the principles and practices outlined above, healthcare professionals can provide high-quality care for patients with pneumothorax requiring chest tube management, leading to improved outcomes and reduced morbidity.