Pre Diabetes Meds
Pre-diabetes is a condition where blood sugar levels are higher than normal but not high enough to be classified as diabetes. It’s a critical stage, as it can precede the development of type 2 diabetes if left untreated. According to the Centers for Disease Control and Prevention (CDC), more than 88 million adults in the United States have pre-diabetes, and 90% of them don’t even know they have it. Managing pre-diabetes through lifestyle changes and, in some cases, medication can significantly reduce the risk of progressing to type 2 diabetes.
Understanding Pre-diabetes
Pre-diabetes, also known as impaired glucose tolerance, indicates that the body is having trouble managing blood glucose levels. This condition can lead to the development of heart disease and type 2 diabetes over time if not properly addressed. The primary goal in managing pre-diabetes is to reduce blood glucose levels to a normal range and prevent the onset of type 2 diabetes.
Lifestyle Changes
Before considering medication, lifestyle changes are the first line of defense against pre-diabetes. These include:
- Dietary Changes: Eating a balanced diet that is low in sugar, salt, and unhealthy fats. Focusing on whole foods like vegetables, fruits, whole grains, lean proteins, and healthy fats can help manage blood sugar levels.
- Physical Activity: Regular physical activity, such as walking, can help improve insulin sensitivity, which is the body’s ability to effectively use insulin.
- Weight Management: Losing weight, if needed, can help improve insulin sensitivity and reduce the risk of developing type 2 diabetes.
- Quit Smoking: Smoking can increase the risk of developing type 2 diabetes, so quitting is highly recommended.
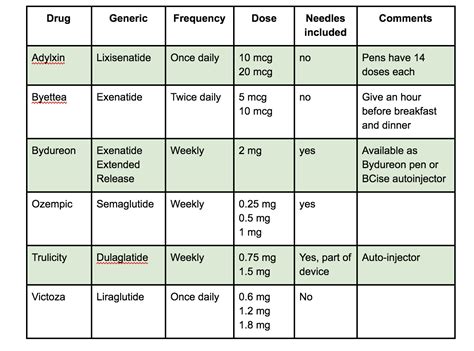
Medications for Pre-diabetes
While lifestyle changes are the cornerstone of managing pre-diabetes, in some cases, healthcare providers may prescribe medications to help regulate blood sugar levels and improve insulin sensitivity. The decision to use medication depends on various factors, including the presence of other health conditions, the severity of pre-diabetes, and how well lifestyle changes are working.
Metformin: This is the most commonly prescribed medication for pre-diabetes. Metformin works by decreasing glucose production in the liver, improving the body’s sensitivity to insulin, and thereby facilitating the uptake of glucose by cells. It’s particularly recommended for individuals with pre-diabetes who are at high risk of developing type 2 diabetes, such as those with a high body mass index (BMI), a history of gestational diabetes, or those who have multiple risk factors for cardiovascular disease.
Pioglitazone: Though not as commonly used for pre-diabetes as metformin, pioglitazone can improve insulin sensitivity. However, its use is less frequent due to potential side effects, such as fluid retention and an increased risk of heart failure.
Orlistat: This drug helps with weight loss by reducing the absorption of fats from the human diet, thereby aiding in weight management, which is crucial for individuals with pre-diabetes.
Future Directions in Managing Pre-diabetes
Research continues to uncover new approaches to managing pre-diabetes. For instance, there’s growing interest in the potential benefits of certain nutrients and dietary patterns, such as the Mediterranean diet, which may help improve insulin sensitivity. Additionally, studies are exploring the role of pharmacological agents that target different pathways involved in glucose metabolism, offering hope for more effective therapeutic options in the future.
Proactive Management
Managing pre-diabetes requires a proactive approach. Regular monitoring of blood glucose levels and working closely with a healthcare provider to adjust treatment plans as necessary are key components of successful management. Moreover, understanding the importance of early intervention can motivate individuals to make critical lifestyle changes and adhere to medication regimens if prescribed.
Decision Framework for Medication Use
The decision to use medication for pre-diabetes involves careful consideration of several factors:
- Risk of Progression: The risk of progressing to type 2 diabetes.
- Presence of Other Conditions: Such as hypertension, high cholesterol, or heart disease.
- Response to Lifestyle Changes: How well the individual responds to dietary changes, increased physical activity, and weight loss.
- Potential Side Effects: Weighing the benefits of medication against potential side effects.
Conclusion
Pre-diabetes is a critical health condition that requires immediate attention. Through a combination of lifestyle changes and, when necessary, medication, individuals can significantly reduce their risk of developing type 2 diabetes and related health issues. Early intervention and a proactive approach to health management are crucial for preventing the progression of pre-diabetes to type 2 diabetes.
What are the primary lifestyle changes recommended for managing pre-diabetes?
+The primary lifestyle changes include adopting a balanced diet low in sugar and unhealthy fats, engaging in regular physical activity, managing weight, and quitting smoking if applicable. These changes can help improve insulin sensitivity and reduce the risk of developing type 2 diabetes.
What medication is commonly prescribed for pre-diabetes, and how does it work?
+Metformin is the most commonly prescribed medication for pre-diabetes. It works by decreasing glucose production in the liver, improving the body’s sensitivity to insulin, and facilitating the uptake of glucose by cells. This helps in managing blood sugar levels and reducing the risk of developing type 2 diabetes.
What factors are considered when deciding to use medication for pre-diabetes?
+The decision to use medication involves considering the risk of progressing to type 2 diabetes, the presence of other health conditions, the individual’s response to lifestyle changes, and the potential side effects of the medication. A healthcare provider weighs these factors to determine the best course of action.