Retinal Detachment Surgery: Repair Guide
The delicate retina, a layer of tissue at the back of the eye, plays a crucial role in vision by converting light into signals sent to the brain. However, when the retina detaches from its normal position, it can lead to severe vision loss if not treated promptly. Retinal detachment surgery is a complex procedure designed to repair this condition, and understanding the process, risks, and outcomes is essential for individuals facing this challenge.
Understanding Retinal Detachment
Before diving into the surgical aspects, it’s vital to comprehend what retinal detachment is and how it occurs. The retina can detach from the back of the eye due to a tear or hole, allowing fluid to seep underneath and separate the retina from its underlying tissue. This can result from trauma, diabetic retinopathy, tumors, or as a complication of other eye surgeries. Symptoms may include sudden flashes of light, an increase in eye floaters, and a curtain or shadow descending over the field of vision.
Pre-Surgical Preparation
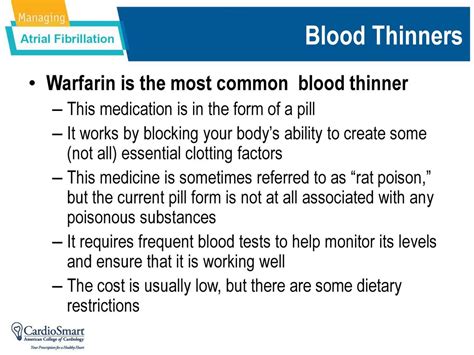
The journey to retinal detachment surgery begins with a comprehensive diagnostic examination. An eye care professional will use specialized equipment to examine the retina, often using optical coherence tomography (OCT) or ultrasound to assess the extent of the detachment. Patients are then prepared for surgery, which may involve stopping certain medications, especially those that thin the blood, to reduce the risk of bleeding during the procedure.
Surgical Techniques
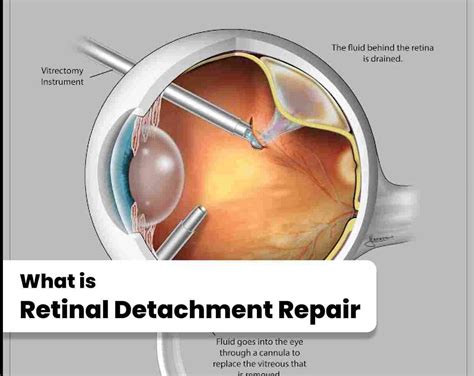
Several surgical techniques can be employed to repair a detached retina, with the choice depending on the size and location of the detachment, as well as the surgeon’s preference. The primary goal is to close any tears or holes and ensure the retina is reattached to its proper position.
Scleral Buckling Surgery: This involves placing a flexible band around the eye to counteract the force pulling the retina out of place. The band pushing on the eye wall helps to close the retinal tear and may be left in place permanently.
Vitrectomy: In this procedure, the vitreous gel is removed and replaced with a gas or oil to help the retina reattach. Over time, the body replaces the gas or oil with its natural fluids.
Pneumatic Retinopexy: A less invasive procedure where a gas bubble is injected into the vitreous space. The bubble pushes against the detached retina, helping it to reattach. Patients must maintain a specific head position for a while to ensure the bubble is in the correct position.
Post-Surgical Care
After surgery, patients typically experience some discomfort, redness, and vision blurriness, which can be managed with medication. It’s crucial to follow the post-operative instructions carefully, including any positioning requirements to facilitate the healing process. Regular follow-up appointments with the eye care professional are necessary to monitor the healing progress and remove any sutures or gas.
Risks and Complications
As with any surgical procedure, retinal detachment surgery comes with risks and potential complications. These can include infection, cataract formation, increased eye pressure, and vision loss. In some cases, additional surgeries may be required to address these complications or to improve vision outcomes.
Future Outlook and Vision Recovery
The success of retinal detachment surgery can vary, and the extent of vision recovery depends on several factors, including the duration of the detachment, the size of the detachment, and the presence of any underlying conditions. In general, the sooner the surgery is performed, the better the chances of recovering vision. However, even with successful surgery, some visual disturbances may persist.
Conclusion
Retinal detachment surgery is a intricate and delicate procedure aimed at preserving vision and restoring the retina to its normal position. By understanding the causes, surgical techniques, and aftercare involved, individuals can better navigate their treatment journey. It’s a testament to medical advancement that such complex procedures are available, offering hope for those at risk of severe vision loss due to retinal detachment.
What are the symptoms of retinal detachment?
+Symptoms of retinal detachment include sudden flashes of light, an increase in eye floaters, and a curtain or shadow descending over the field of vision.
How long does it take to recover from retinal detachment surgery?
+Recovery time can vary but generally involves several weeks to months. The eye may take some time to heal completely, and regular follow-up appointments are crucial to monitor the healing progress.
Can retinal detachment be prevented?
+While some cases of retinal detachment cannot be prevented, regular eye exams can help identify risk factors such as retinal tears early. Prompt treatment of these conditions can significantly reduce the risk of detachment.