Sacral Bone Fracture
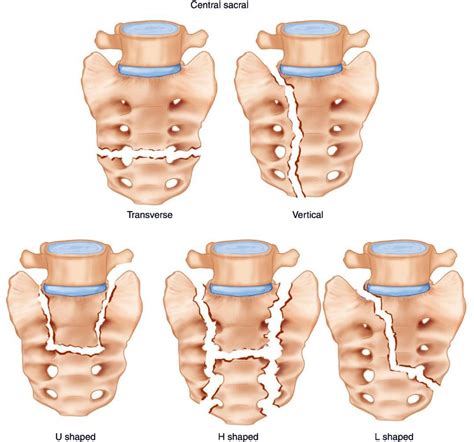
The sacrum, a large, triangular bone located at the base of the spine and the center of the pelvis, plays a crucial role in supporting the spine and pelvis. A sacral bone fracture, also known as a sacral fracture, can be a complex and potentially debilitating injury. This type of fracture can occur due to various reasons, including high-impact trauma, such as a car accident or a fall from a significant height, as well as repetitive stress or overuse, which can lead to stress fractures.
Understanding the anatomy of the sacrum is essential in comprehending the severity and potential complications of a sacral fracture. The sacrum is formed by the fusion of five sacral vertebrae and serves as a foundation for the spine, transmitting forces from the spine to the pelvis. It also forms the base of the pelvic cavity, providing protection for the pelvic organs. A fracture in this area can lead to significant pain, mobility issues, and, in severe cases, neurological symptoms due to compression or damage to the nerves that exit the spinal canal through the sacrum.
Causes and Risk Factors
Several factors can increase the risk of sustaining a sacral bone fracture. These include:
- High-Impact Trauma: The most common cause of sacral fractures is high-impact trauma, such as that sustained in a car accident, a fall from a height, or a direct blow to the pelvis during contact sports.
- Osteoporosis: Individuals with osteoporosis, a condition characterized by weakened bones, are at a higher risk of fractures, including those of the sacrum, due to lesser impact or even without any noticeable trauma.
- Repetitive Stress: Athletes or individuals involved in activities that subject their bones to repetitive stress and impact, such as long-distance runners, are at risk of developing stress fractures in the sacrum.
- Age: With advancing age, the risk of fractures increases due to decreased bone density and the potential for osteoporosis.
Symptoms and Diagnosis
The symptoms of a sacral bone fracture can vary depending on the severity and location of the fracture. Common symptoms include:
- Severe Pain: Pain in the lower back or pelvis that worsens with movement.
- Limited Mobility: Difficulty walking or standing due to pain.
- Neurological Symptoms: Numbness, tingling, or weakness in the legs, indicating nerve compression or damage.
Diagnosing a sacral fracture typically involves a combination of physical examination, medical history, and imaging studies. Imaging tests such as X-rays, CT scans, or MRI scans are used to confirm the presence and extent of the fracture. In some cases, a bone scan may be recommended to detect stress fractures or other bone abnormalities.
Treatment Options
The treatment of a sacral bone fracture depends on the type and severity of the fracture, as well as the overall health of the individual. Treatment options can range from conservative management to surgical intervention.
- Conservative Management: For less severe fractures, treatment may involve bed rest, pain management with medication, and gradual mobilization. In cases of stress fractures, activities that exacerbate the condition may need to be avoided for a period.
- Surgical Intervention: For more severe fractures, especially those that involve displacement of the bone fragments or neurological symptoms, surgery may be necessary. The goal of surgery is to stabilize the fracture, relieve pressure on the nerves, and restore the normal anatomy of the pelvis and spine.
Recovery and Rehabilitation
Recovery from a sacral bone fracture can be a lengthy process, especially if surgical intervention is required. A comprehensive rehabilitation program, including physical therapy, is crucial for restoring strength, flexibility, and range of motion. The rehabilitation process should be tailored to the individual’s specific needs and the severity of the fracture.
In addition to formal rehabilitation programs, making lifestyle adjustments can aid in the recovery process. This includes maintaining a healthy diet rich in calcium and vitamin D to support bone healing, engaging in low-impact exercises to maintain mobility without exacerbating the fracture, and avoiding smoking and excessive alcohol consumption, which can impede the healing process.
Complications and Long-Term Implications
While many individuals can recover fully from a sacral bone fracture, there are potential complications and long-term implications to consider. These include:
- Chronic Pain: Some individuals may experience chronic pain, which can significantly impact quality of life.
- Neurological Deficits: In cases where the fracture compresses or damages nerves, there may be long-term neurological symptoms such as numbness, tingling, or weakness in the legs.
- Arthritis: Fractures that involve the joints of the pelvis can lead to the development of arthritis over time, resulting in chronic pain and stiffness.
- Osteoporosis: Individuals who sustain a fracture due to osteoporosis are at increased risk of future fractures, making ongoing management of bone health crucial.
In conclusion, a sacral bone fracture is a significant injury that requires prompt and appropriate treatment to prevent long-term complications. Understanding the causes, symptoms, and treatment options for sacral fractures can help individuals seek medical attention early and make informed decisions about their care. With advancements in medical technology and rehabilitation techniques, many individuals can make a full recovery from a sacral bone fracture and return to their normal activities.
What are the primary causes of sacral bone fractures?
+The primary causes of sacral bone fractures include high-impact trauma, such as car accidents or falls, repetitive stress from activities like long-distance running, and weakened bones due to conditions like osteoporosis.
How are sacral bone fractures diagnosed?
+Diagnosis typically involves a physical examination, review of medical history, and imaging studies such as X-rays, CT scans, or MRI scans to confirm the presence and extent of the fracture.
What are the treatment options for sacral bone fractures?
+Treatment options depend on the severity of the fracture and can range from conservative management with bed rest and pain medication to surgical intervention to stabilize the fracture and relieve pressure on nerves.
Can sacral bone fractures lead to long-term complications?
+Yes, potential long-term complications include chronic pain, neurological deficits, arthritis, and an increased risk of future fractures, especially in individuals with osteoporosis.