Small Bowel Obstruction Symptoms
The small bowel, also known as the small intestine, plays a crucial role in the digestive process. It is responsible for absorbing nutrients from the food we eat, and any disruption in its function can lead to severe complications. One such disruption is a small bowel obstruction, which occurs when the normal flow of intestinal contents is blocked, preventing the normal movement of food, fluid, and gas. This condition requires immediate medical attention, as it can lead to serious consequences, including tissue death, infection, and even death if left untreated.
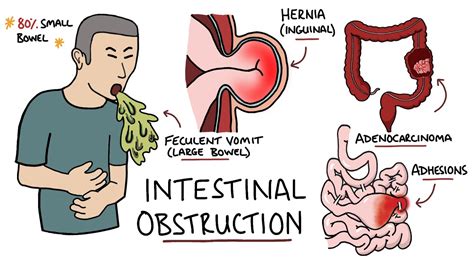
The symptoms of small bowel obstruction can vary depending on the severity and location of the blockage, but there are common signs that individuals should be aware of. One of the earliest and most common symptoms is abdominal pain, which can range from mild to severe. This pain often comes and goes, and its intensity can increase over time. Another frequent symptom is vomiting, which may start as vomiting food and later progress to vomiting bile or fecal matter. Nausea often accompanies vomiting, further complicating the digestive process.
Bloating and abdominal distension are also prevalent, as the bowel becomes filled with fluid and gas. Individuals may experience constipation, as the obstruction prevents normal bowel movements, or they might have diarrhea, depending on the location and nature of the blockage. The abdomen may become tender to the touch, and in severe cases, a fever can develop due to infection.
In some cases, especially if the obstruction is partial or the individual has had previous abdominal surgery, the symptoms might be less severe or misleading, making diagnosis more challenging. For instance, some people may experience mild cramping or intermittent abdominal discomfort without severe vomiting or constipation, leading them to delay seeking medical help.
It’s crucial to recognize the risk factors for small bowel obstruction to understand who might be more susceptible. Previous abdominal surgery is a significant risk factor, as adhesions from the surgery can lead to obstructions. Hernias, inflammatory bowel diseases like Crohn’s disease, and tumors (either benign or malignant) can also cause blockages. Less commonly, conditions such as intussusception, where a part of the intestine telescopes into another part, or volvulus, a twisting of the intestine, can lead to obstruction.
Diagnosing small bowel obstruction often involves a combination of physical examination, medical history, and imaging studies. A physician will typically start by reviewing the patient’s symptoms and medical history, looking for clues such as previous surgeries or conditions that could predispose to an obstruction. A physical examination can reveal abdominal tenderness, guarding (muscle tension), and distension.
Imaging studies are critical in confirming the diagnosis and determining the cause and severity of the obstruction. X-rays can show signs of obstruction, such as air-fluid levels in the small bowel, and can help identify any free air under the diaphragm, which would indicate a perforation. Computed Tomography (CT) scans provide more detailed information about the location of the obstruction, its cause, and any complications that may have developed, such as ischemia (lack of blood flow) to the bowel.
Treatment for small bowel obstruction depends on the underlying cause, the severity of the obstruction, and whether there are any complications. In some cases, especially if the obstruction is partial or not causing severe symptoms, conservative management may be attempted. This involves bowel rest (nothing by mouth), intravenous fluids to prevent dehydration, and possibly the use of nasogastric suction to decompress the bowel.
However, many cases require surgical intervention, especially if there’s evidence of bowel ischemia, perforation, or if conservative management fails. Surgery typically involves removing the cause of the obstruction and any portion of the bowel that has been compromised. In some instances, a bowel resection (removal of a segment of the bowel) followed by an anastomosis (reconnection of the bowel) may be necessary.
Preventing small bowel obstruction involves managing risk factors when possible. For individuals with a history of abdominal surgery, following post-operative instructions carefully and attending follow-up appointments can help in early detection of potential complications. Maintaining a healthy lifestyle, managing chronic conditions effectively, and seeking prompt medical attention for any severe or persistent abdominal symptoms can also play a significant role in reducing the risk of complications associated with small bowel obstructions.
What are the common symptoms of small bowel obstruction?
+The common symptoms include abdominal pain, vomiting, nausea, bloating, abdominal distension, constipation, and in some cases, fever. The severity and combination of these symptoms can vary depending on the cause and location of the obstruction.
What are the risk factors for developing small bowel obstruction?
+Prior abdominal surgery, hernias, inflammatory bowel diseases, tumors, and conditions like intussusception or volvulus can increase the risk of small bowel obstruction. Recognizing these risk factors is crucial for early diagnosis and treatment.
How is small bowel obstruction diagnosed?
+Diagnosis involves a combination of physical examination, reviewing medical history, and imaging studies like X-rays and CT scans. These tools help in identifying the cause, location, and severity of the obstruction, as well as detecting any complications.
What are the treatment options for small bowel obstruction?
+Treatment depends on the cause and severity of the obstruction. Conservative management with bowel rest and fluids may be attempted, but many cases require surgical intervention to remove the cause of the obstruction and repair any damaged bowel.
In conclusion, small bowel obstruction is a serious condition that requires prompt recognition and treatment to prevent severe complications. Understanding the symptoms, risk factors, and treatment options can help individuals seek medical care early and improve outcomes. Given the potential for significant morbidity and mortality, it’s crucial for healthcare providers to approach these cases with urgency and a comprehensive management plan.


