Steroids For Asthma

Asthma is a chronic respiratory condition characterized by inflammation, airway obstruction, and spasm of the bronchial tubes, which can lead to recurring episodes of wheezing, chest tightness, shortness of breath, and coughing. The primary goal of asthma management is to control symptoms, improve quality of life, and prevent exacerbations. One of the key treatment options for asthma involves the use of corticosteroids, which are a type of steroid hormone. In this article, we will delve into the world of steroids for asthma, exploring their types, mechanisms, benefits, and potential drawbacks.
Understanding Asthma and Inflammation
Asthma is a complex condition, and its pathophysiology involves multiple cell types, including eosinophils, neutrophils, mast cells, and T lymphocytes, which contribute to airway inflammation. This inflammation leads to the production of various cytokines, chemokines, and other mediators, causing airway hyperresponsiveness, remodeling, and obstruction. Corticosteroids have potent anti-inflammatory effects, which make them an essential component of asthma therapy.
Types of Steroids for Asthma
There are several types of corticosteroids used to treat asthma, including:
- Inhaled Corticosteroids (ICS): These are the most commonly used steroids for asthma. ICS are administered directly to the lungs using an inhaler, reducing the risk of systemic side effects. Examples of ICS include fluticasone, budesonide, and beclomethasone.
- Oral Corticosteroids: These are used for acute asthma exacerbations or for patients with severe asthma. Oral corticosteroids, such as prednisone, are usually prescribed for a short period (e.g., 5-7 days) to quickly reduce inflammation.
- Systemic Corticosteroids: These are used in severe asthma cases, where the patient requires hospitalization. Systemic corticosteroids, like methylprednisolone, are administered intravenously to rapidly control inflammation.
Mechanisms of Action
Corticosteroids exert their effects by:
- Reducing Inflammation: Corticosteroids decrease the production of inflammatory cytokines and chemokines, leading to a reduction in airway inflammation.
- Inhibiting Airway Remodeling: Corticosteroids prevent the deposition of collagen and other matrix proteins, which can lead to airway remodeling and obstruction.
- Improving Airway Hyperresponsiveness: Corticosteroids reduce the sensitivity of airway smooth muscle to various stimuli, thereby decreasing airway hyperresponsiveness.
Benefits of Steroids for Asthma
The use of corticosteroids in asthma management offers several benefits, including:
- Improved Symptom Control: Corticosteroids reduce symptoms of asthma, such as wheezing, coughing, and shortness of breath.
- Reduced Exacerbations: Regular use of ICS can decrease the frequency and severity of asthma exacerbations.
- Improved Quality of Life: By controlling symptoms and reducing exacerbations, corticosteroids can significantly improve the quality of life for asthma patients.
- Reduced Mortality: The use of corticosteroids has been associated with a decreased risk of asthma-related mortality.
Potential Drawbacks and Side Effects
While corticosteroids are effective in managing asthma, they can also have potential drawbacks and side effects, including:
- Local Side Effects: ICS can cause local side effects, such as oral thrush, hoarseness, and coughing.
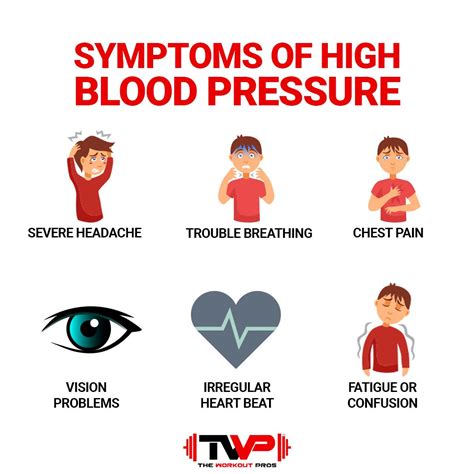
- Systemic Side Effects: Oral and systemic corticosteroids can cause systemic side effects, such as weight gain, mood changes, and increased blood pressure.
- Bone Density Loss: Long-term use of oral corticosteroids can lead to bone density loss and osteoporosis.
- Adrenal Suppression: Prolonged use of systemic corticosteroids can suppress the adrenal glands, leading to adrenal insufficiency.
Future Directions and Emerging Therapies
The development of new therapeutic agents and the refinement of existing treatments continue to improve asthma management. Some emerging therapies, such as biologics and small molecule inhibitors, target specific molecular pathways involved in airway inflammation and remodeling. These innovative approaches may offer improved efficacy and safety profiles compared to traditional corticosteroids.
What is the primary mechanism of action of corticosteroids in asthma?
+Corticosteroids primarily reduce inflammation in the airways by decreasing the production of inflammatory cytokines and chemokines.
What are the potential side effects of long-term inhaled corticosteroid use?
+Long-term use of inhaled corticosteroids can lead to local side effects, such as oral thrush and hoarseness, as well as systemic side effects, including bone density loss and adrenal suppression.
Can corticosteroids be used to treat acute asthma exacerbations?
+Yes, oral or systemic corticosteroids can be used to treat acute asthma exacerbations, reducing inflammation and rapidly improving symptoms.
In conclusion, corticosteroids play a vital role in managing asthma by reducing inflammation, improving symptom control, and decreasing the risk of exacerbations. While they have potential drawbacks and side effects, the benefits of corticosteroid therapy can be maximized by carefully selecting the most effective treatment regimen and monitoring patients closely. As research continues to uncover the complexities of asthma pathophysiology, the development of innovative therapies and the refinement of existing treatments will further improve patient outcomes.